Humana Prior Authorization Form 2024 - At Humana we are dedicated to ensuring every business decision we make reflects our commitment to improving the health and well being of our members To that end we continuously 2024 These are deleted codes effective Jan 1 2024 Prosthetics L7185 L7186 L7190 L7191 Removed Nov 17 2023 Jan 1 2024 These codes will be removed from
Humana has enhanced its approval process on the Availity web portal with a new preauthorization automation feature This optional feature can provide immediate determinations for requests that previously may have been pended for review How it works
Humana Prior Authorization Form 2024
Humana Prior Authorization Form 2024
Your doctor or healthcare provider can submit inpatient and outpatient referral, prior authorization and preauthorization requests online through our provider portal. or via Humana.com. Once here, they can submit a new request or update an existing request. They can also contact our Clinical Intake team at 800 - 523 - 0023. .
We require the following data to make a decision your name and the member ID from your Humana ID card an itemized statement from the provider showing the services provided with the date s of service for those services and your receipt or other proof of your payment
Provider Preauthorization Tool Humana
Y0040 GHHLYL3EN M 2024 DEN478 278501ALL0723 A Page 1 of 20 The following provides an all inclusive list of dental services covered under this plan Limitations and exclusions Members For information about your dental benefits call Humana Dental Customer Service at 800 457 4708 TTY 711 Monday Friday 8 a m 6 p m in your time
Covermymeds Humana Prior Auth Form Bcbs Prior Authorization Form Medication Form Resume
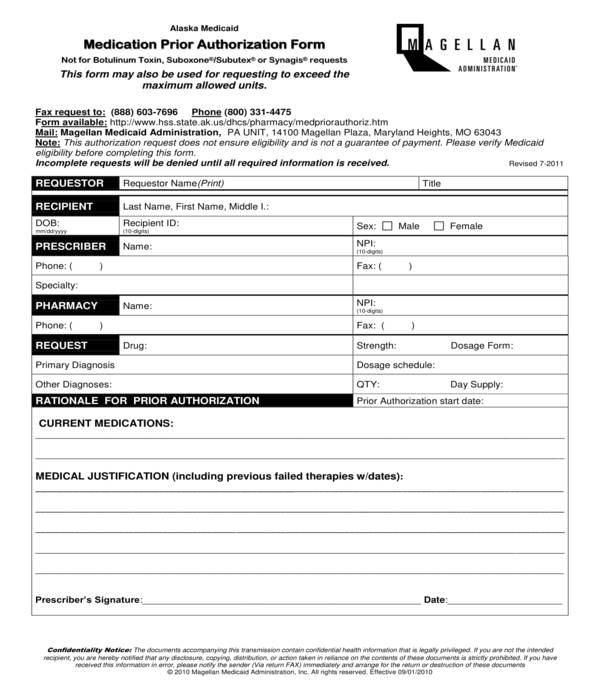
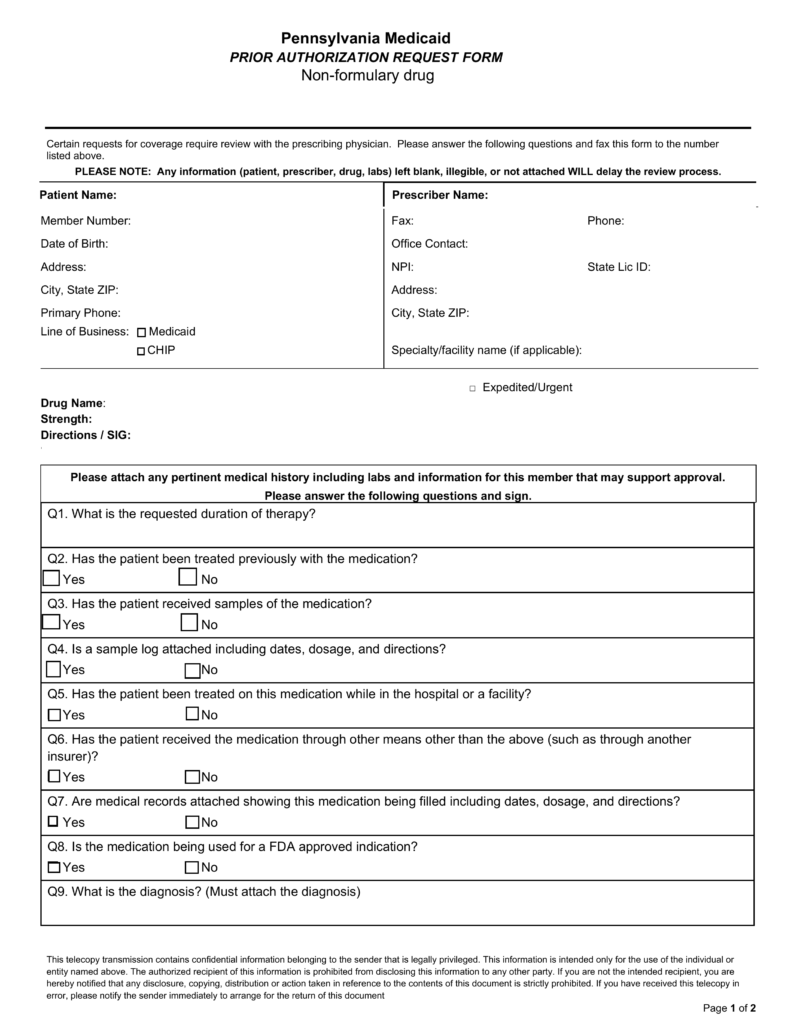
By submitting this form the pharmacist may be able to have the medication covered by Humana In your form you will need to explain your rationale for making this request including a clinical justification and referencing any relevant lab test results Fax 1 800 555 2546 Phone 1 877 486 2621 Humana Universal Prior Authorization Form
Covermymeds Humana Prior Auth Form Humana Prior Authorization Form Unique Authorization
Covermymeds Humana Prior Auth Form Form Resume Examples bX5aVMLOwW
Commercial Summary Of Medical Preauthorization And Humana
Follow these easy steps to become Humana Medicare member Have your Medicare card ready Each individual applying must fill out separate form Sign and date the enrollment form If the enrollment form is not completed and returned within the allotted time period the enrollment could be denied Submit your enrollment form
Covermymeds Humana Prior Auth Form Key covermymeds Prior Authorization Form Vincegray2014
Please call our Member Services number at 1 800 794 5907 Hours of operation October 1 March 31 7 days a week 8 a m to 8 p m April 1 September 30 Monday Friday 8 a m to 8 p m You may leave a voicemail after hours Saturdays Sundays and holidays and we will return your call within one business day
You can access these plan documents any time by signing into your Humana online profile or by filling out the form below. You can view your plan's provider and pharmacy directory or Drug List online:
How Do I Request A Prior Authorization Or Preauthorization
The Availity Provider Portal is a multi payer site where you can use a single user ID and password to work with Humana and other participating payers online Availity is compliant with all HIPAA regulations and there is no cost to register If you are not registered for the Availity Portal please register here so you have access to the most up to date resources and tools for working with Humana

Covermymeds Humana Prior Auth Form 3 Metzger Snate1989
Humana Medicare Advantage Prior Authorization Forms Form Resume Examples 7mk9MJmkGY
Humana Prior Authorization Form 2024
Please call our Member Services number at 1 800 794 5907 Hours of operation October 1 March 31 7 days a week 8 a m to 8 p m April 1 September 30 Monday Friday 8 a m to 8 p m You may leave a voicemail after hours Saturdays Sundays and holidays and we will return your call within one business day
Humana has enhanced its approval process on the Availity web portal with a new preauthorization automation feature This optional feature can provide immediate determinations for requests that previously may have been pended for review How it works

Humana Prior Authorization Form Pdf Fill Out Sign Online DocHub
Covermymeds Humana Prior Auth Form 2 In Each Of The Below Linked Racingduffer
Bcbs Prior Authorization Form Ohio Form Resume Examples NEpDLPEDxR

Covermymeds Humana Prior Auth Form Printable Optumrx Prior Authorization Appeal Form To
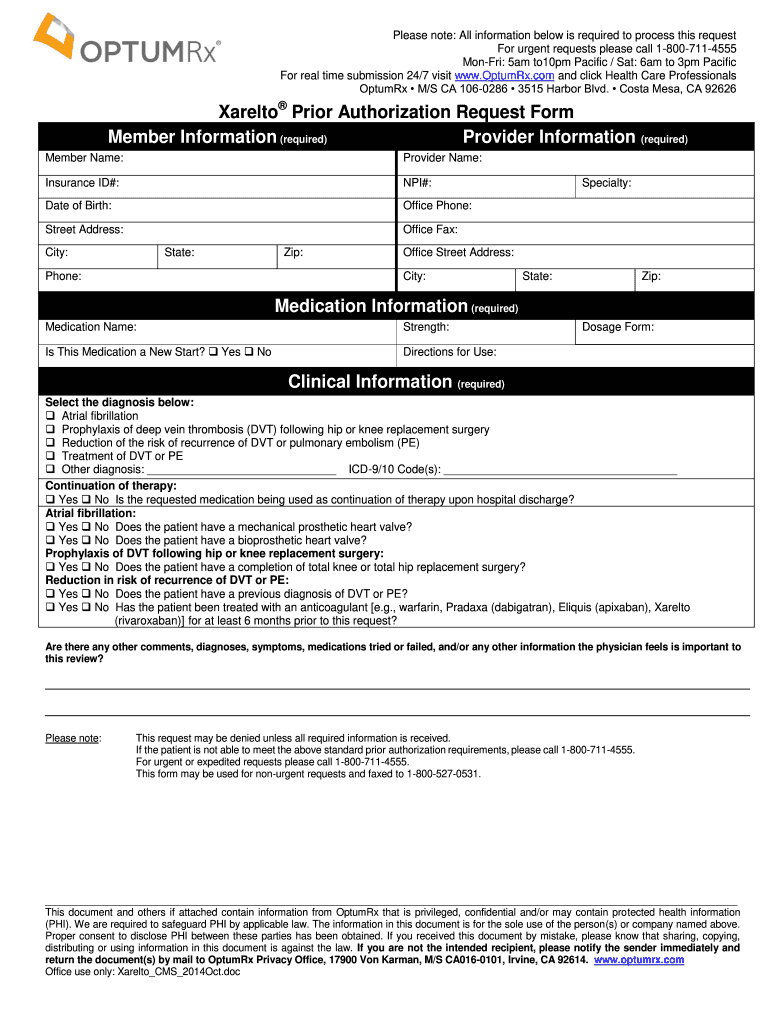
Optumrx Prior Auth Form 2020 2021 Fill And Sign Printable Template Online US Legal Forms