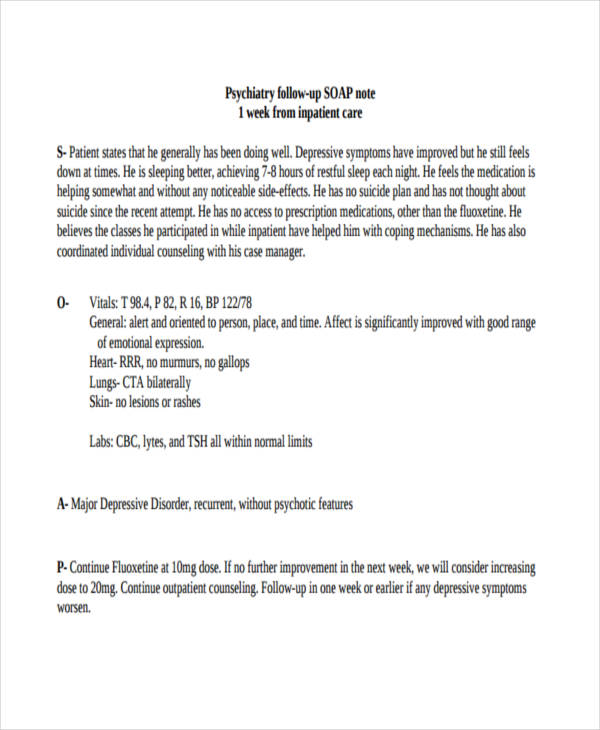
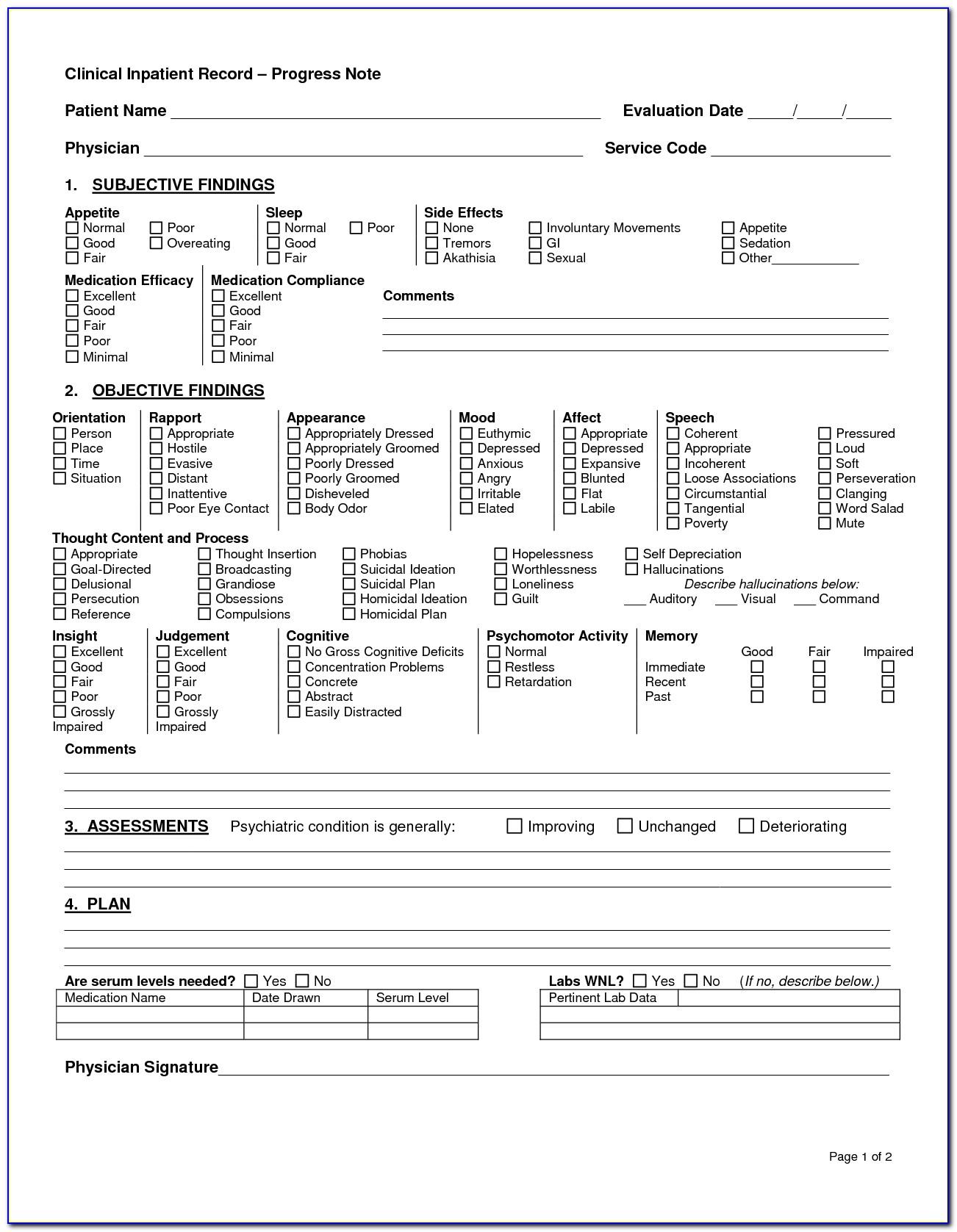
Psychiatry Soap Note Template - Follow up SOAP Note Template for Psychiatrists This template is used for documenting follow up visits with patients The SOAP Subjective Objective Assessment and Plan format is commonly used in medical documentation and includes information about the patient s symptoms a mental status examination an assessment of the patient s
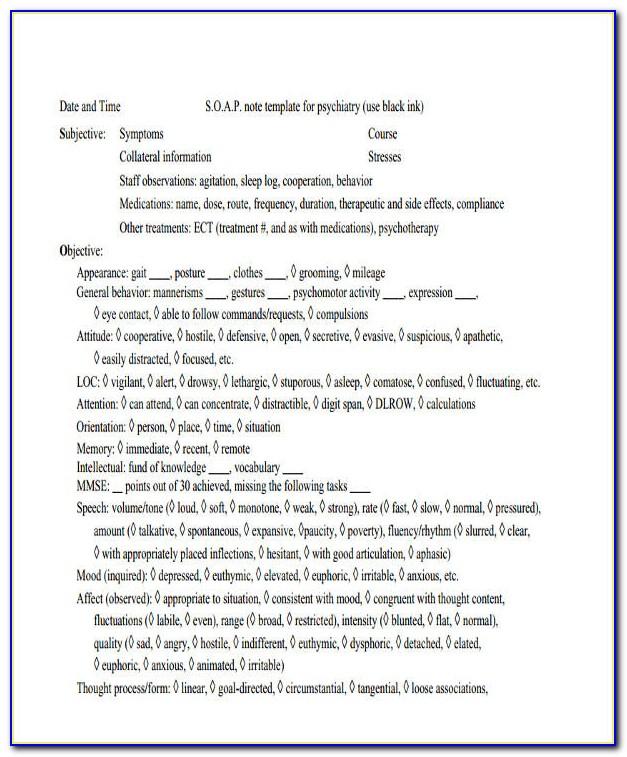
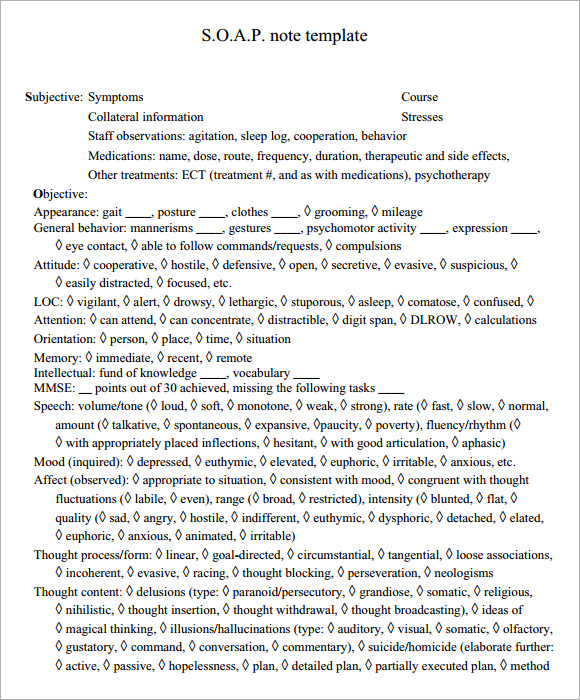
SOAP Subjective Objective Assessment and Plan notes are a structured method for documenting patient information and creating a treatment plan in psychiatric mental health nurse practice This guide provides a thorough overview of SOAP notes their purpose and essential elements tailored for PMHNPs
Psychiatry Soap Note Template
Psychiatry Soap Note Template
In this post, we will review what SOAP notes are, how to write a SOAP note, tips for effective SOAP notes, and a template you can use for your SOAP notes. Download Our comprehensive SOAP Note PDF Template for mental health professionals and other medical professionals for easy note taking and digital storage of client notes:
Our psychiatry SOAP Notes template is specially designed for psychiatrists to document their clinical notes in an efficient and structured way Psychiatrists can use Carepatron s simple to use psychiatry SOAP Notes template to ensure their notes meet the internationally recognized SOAP format
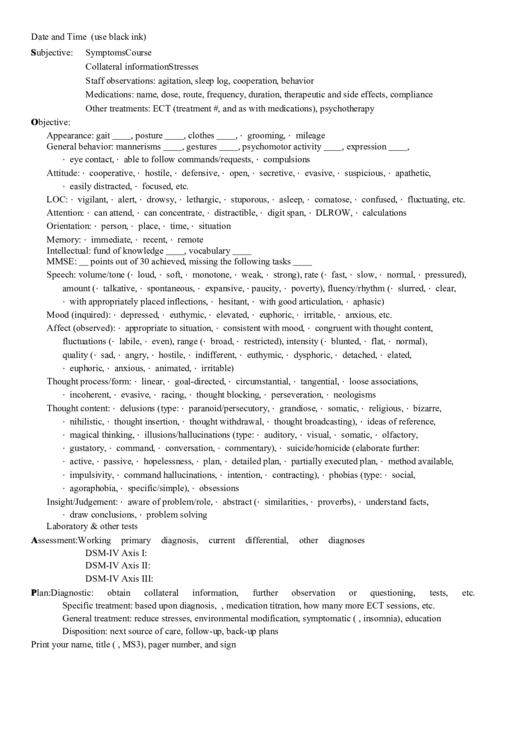
How To Write A Soap Note By PMHNP Helper Substack
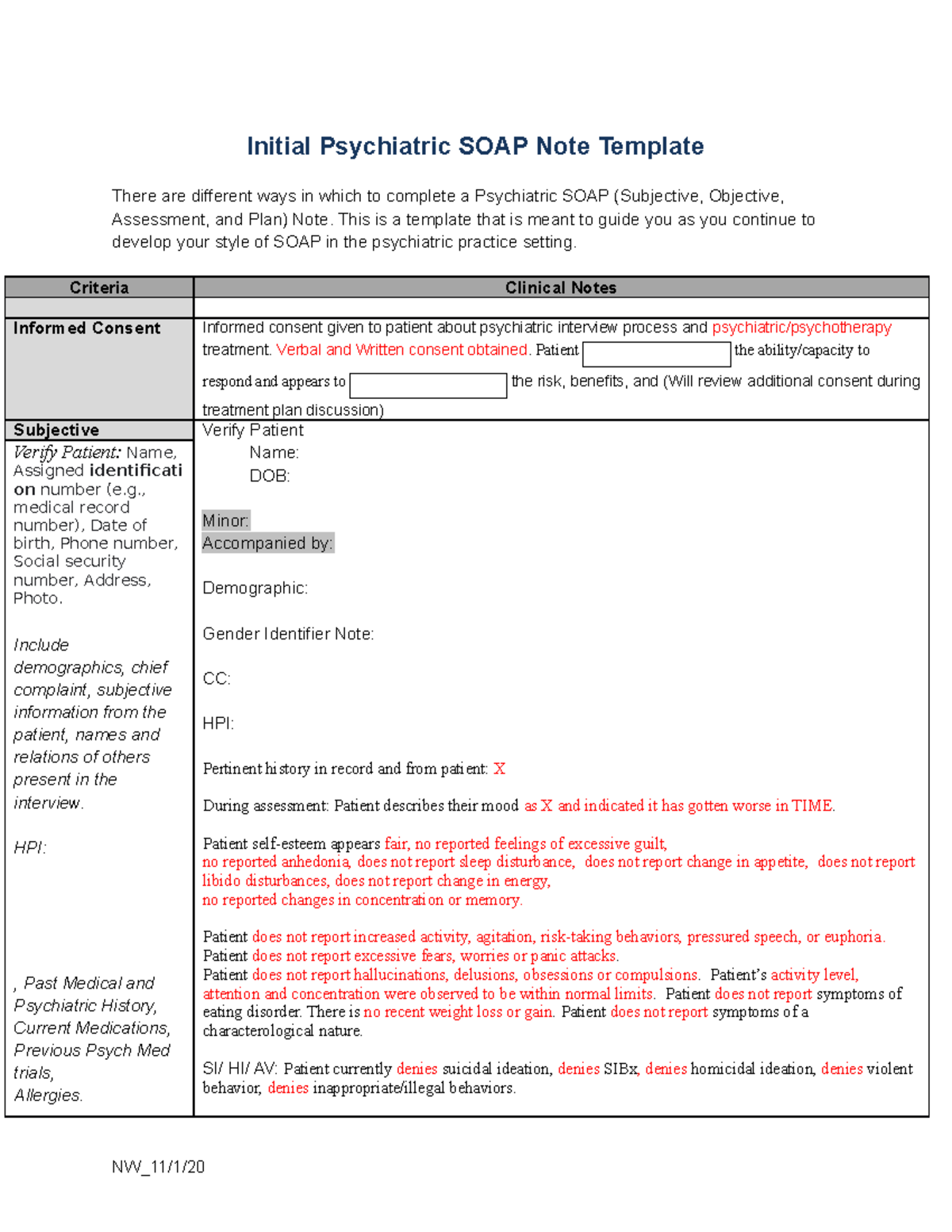
Initial Psychiatric SOAP Note Template There are different ways in which to complete a Psychiatric SOAP Subjective Objective Assessment and Plan Note This is a template that is meant to guide you as you continue to develop your style of SOAP in the psychiatric practice setting
Psychiatry Progress Note Sample
In Psychiatry we often document a patient s current condition and progress in treatment with SOAP notes As you know SOAP stands for the areas of documentation that are considered vital components in order to achieve our goals with treatment In Psychiatry some of the specifics may be unique however the structure of the information and its
FREE 8 Sample Soap Note Templates In MS Word PDF
SOAP Note Examples 19 In PDF Examples
12 Psychiatry Note Templates That Cut Your Documentation
Psychiatry follow up SOAP note 1 week from inpatient care S Patient states that he generally has been doing well Depressive symptoms have improved but he still feels down at times He is sleeping better achieving 7 8 hours of restful sleep each night He feels the medication is helping somewhat and without any noticeable side effects
Psychiatry Soap Note Template
Free SOAP notes templates Medical software tools with built in SOAP notes templates Start saving time with SOAP notes templates SOAP notes document details from patient visits and let you communicate vital information to other healthcare providers Download them for free from the websites mentioned in this article
Psychiatry is a medical specialty that focuses on the workup, treatment, and prevention of various mental disorders, which affect mood, cognition, perception, and behavior. Mental health issues affect approximately 1 in 5 adults and 1 in 6 young people aged 6–17 in the US each year. So a basic understanding of psychiatric conditions and.
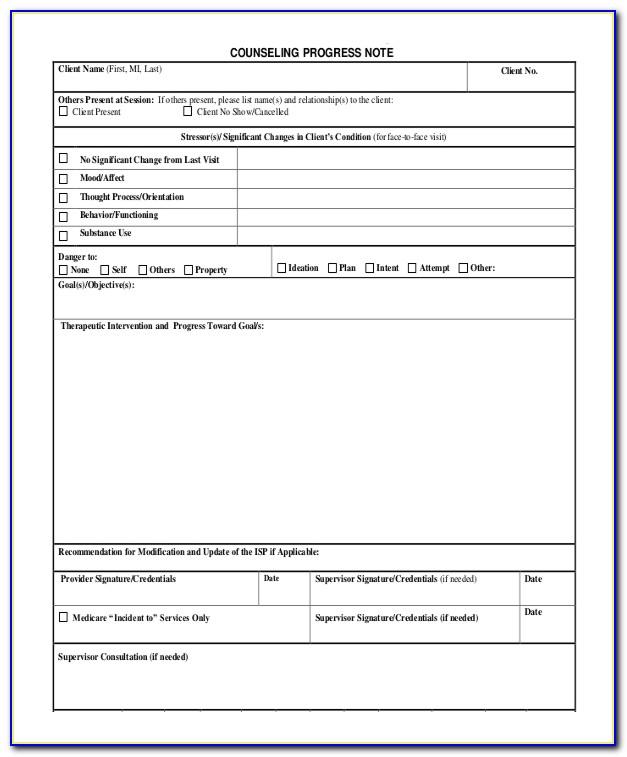
Comprehensive SOAP Notes For Counseling Editable PDF Template
Here s how to write SOAP notes Learning how to write a SOAP note can be one of the most effective ways for clinicians to track assess diagnose and treat clients Here s how to write SOAP notes

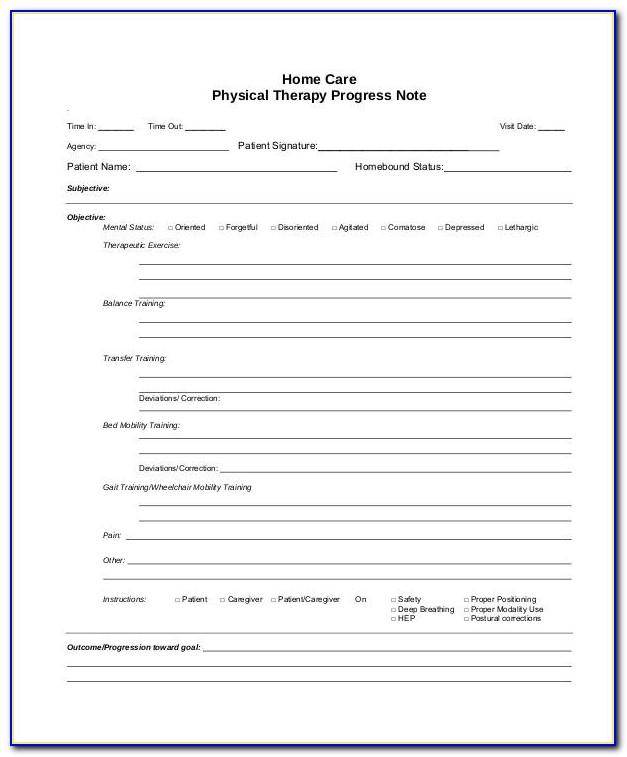
10 Soap Note Template Free Download Word Excel PDF Format

10 Soap Note Template Free Download Word Excel PDF Format
Psychiatry Soap Note Template
Free SOAP notes templates Medical software tools with built in SOAP notes templates Start saving time with SOAP notes templates SOAP notes document details from patient visits and let you communicate vital information to other healthcare providers Download them for free from the websites mentioned in this article
SOAP Subjective Objective Assessment and Plan notes are a structured method for documenting patient information and creating a treatment plan in psychiatric mental health nurse practice This guide provides a thorough overview of SOAP notes their purpose and essential elements tailored for PMHNPs
Psychiatric Soap Note Template

Lactation Consultant Soap Note Sample
Psychiatry Consult Note Template

Dental Soap Note Template
S o a p Note Template For Psychiatry Printable Pdf Download