Allwell Prior Auth Form - Allwell Outpatient Medicare Authorization Form Expedited OUTPATIENT MEDICARE requests Call 1 877 935 8024 Standard Requests Fax to 1 877 687 1183 AUTHORIZATION FORM Request for additional units Existing Authorization Units For Standard requests complete this form and FAX to 1 877 687 1183
2024 Information 2023 Information Prior Authorization Rules for Medical Benefits What is Prior Authorization Prior Authorization is a request made by you or your doctor to get Wellcare By Allwell s approval before receiving treatment
Allwell Prior Auth Form
Allwell Prior Auth Form
Allwell - Inpatient Medicare Authorization Form INPATIENT MEDICARE Expedited Requests: Call 1-844-786-7711 AUTHORIZATION FORM Standard Requests: Fax 1-844-330-7158 Concurrent Requests: Fax 1-844-833-8944 For Standard (Elective Admission) requests, complete this form and FAX to 1-844-330-7158.
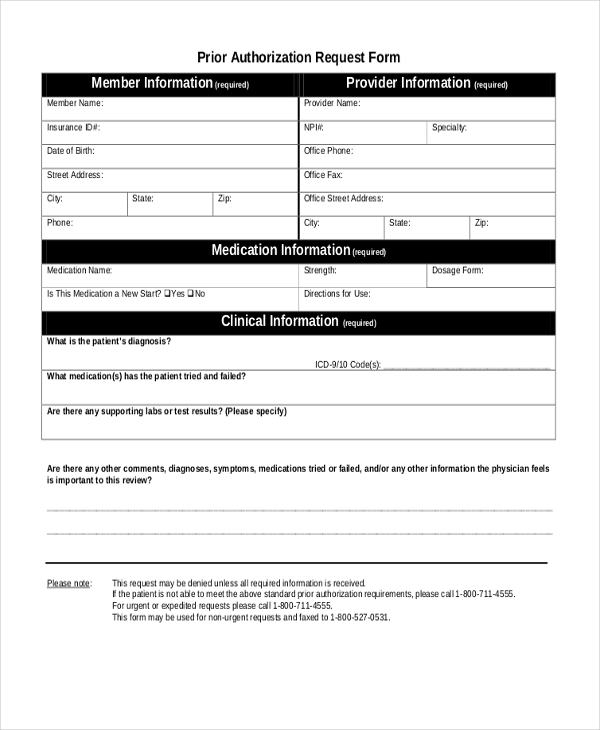
Authorization Forms Delegated Vendor Request Download DME Authorization Request Download Home Health Services Request Download Hospice Authorization Request Download Inpatient Request Download Outpatient Request Download Skilled Therapy Services OT PT ST Prior Authorization Download Surgery Authorization Request Download
Prior Authorization Rules For Medical Benefits Allwell From Superior
All attempts are made to provide the most current information on the Pre Auth Needed Tool However this does NOT guarantee payment Payment of claims is dependent on eligibility covered benefits provider contracts correct coding and billing practices For specific details please refer to the Medicare Advantage provider manual
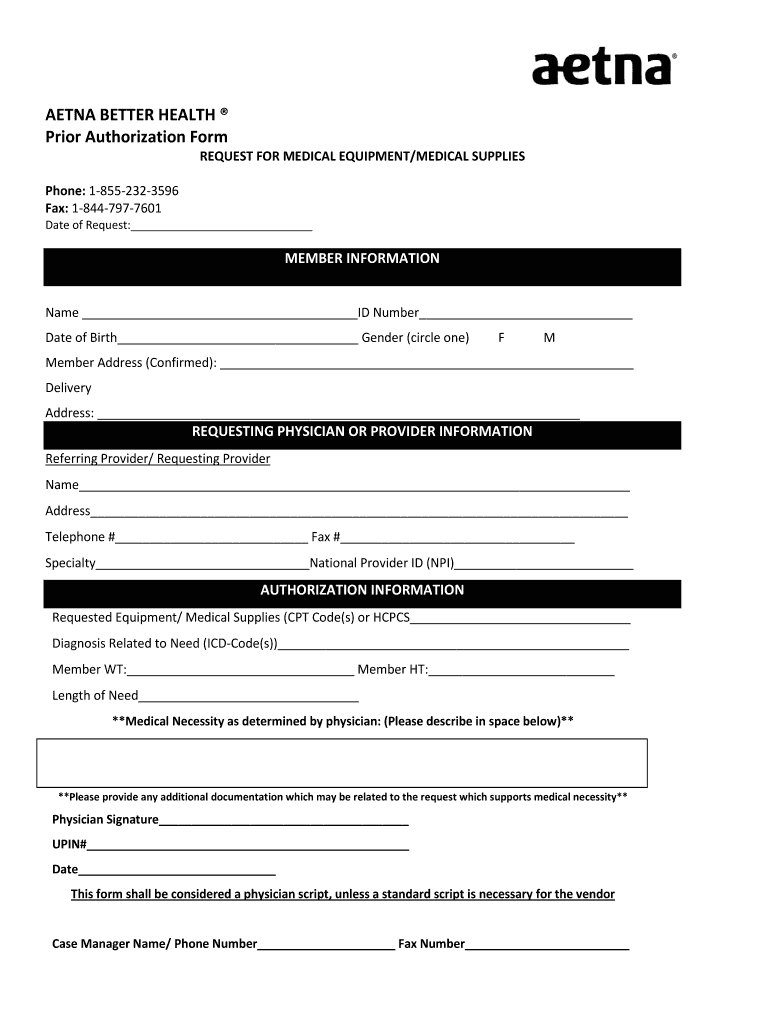
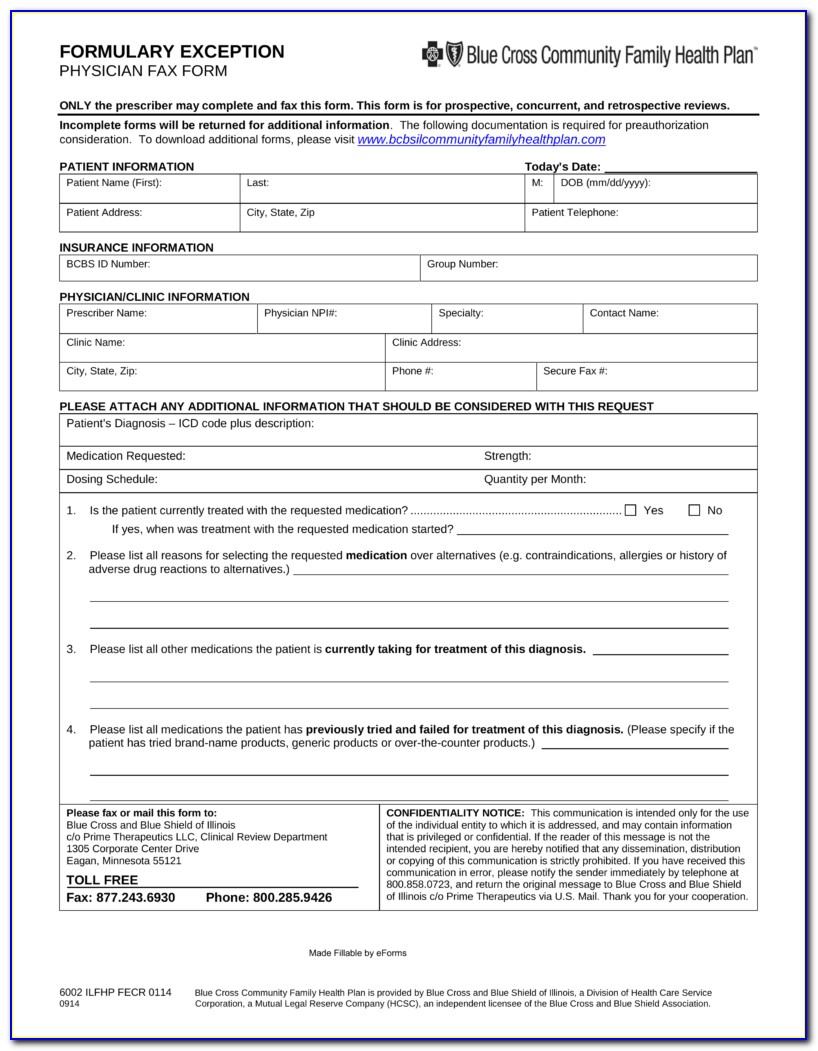
Aetna Better Health Of Wv Prior Auth Form The Gray Tower
AUTHORIZATION FORM Request for additional units Existing Authorization Units For Standard requests complete this form and FAX to 1 844 429 2588 Determination made as expeditiously as the enrollee s health condition requires but no later than 14 calendar days after receipt of request For Expedited requests please CALL 1 855 848 6940
Virginia Department Of Education Prior Authorization Form Pdf Fillable Printable Forms Free Online
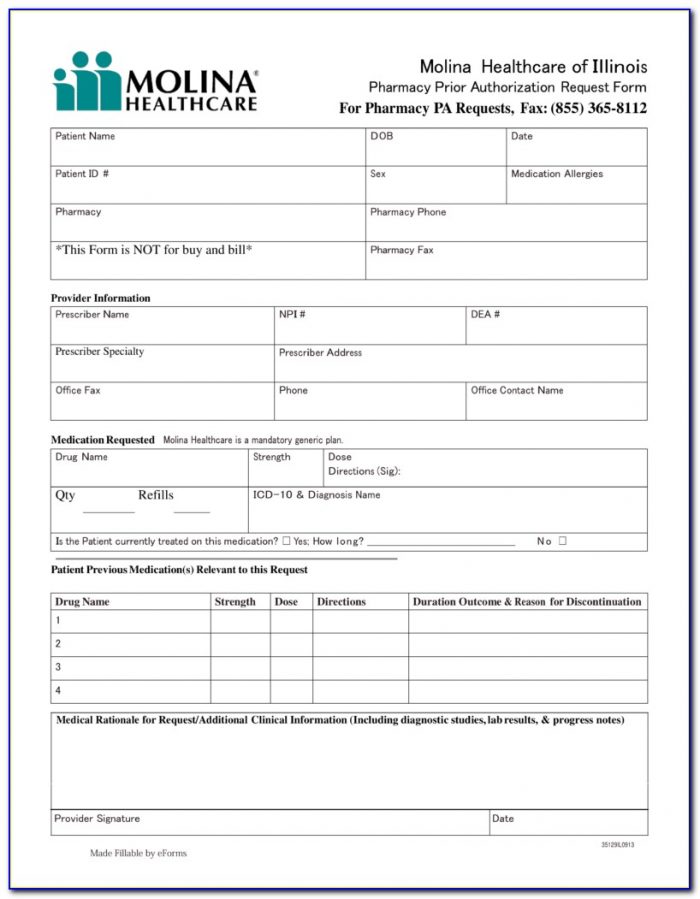
Molina Prior Authorization Request Form Fill Online
Span Class Result Type
Here s a list of pharmacy documents and forms you may need when using your Medicare Part D benefit If you have questions about these items please contact Member Services We re here to help Express Scripts Mail Order Form English PDF last updated Dec 1 2023 Express Scripts Mail Order Form Spanish PDF last updated Dec 1 2023

2023 Wellcare By Allwell Products
Wellcare by Allwell Pre Auth DISCLAIMER All attempts are made to provide the most current information on the Pre Auth Needed Tool However this does NOT guarantee payment Payment of claims is dependent on eligibility covered benefits provider contracts correct coding and billing practices
Use our secure provider portal to submit your Medicaid and Marketplace prior authorization (PA) requests. Your PA request will feed directly into our system and allow us to receive and respond faster. Go to azcompletehealth.com/ then "Login" to register or log in. Opioid Use Disorder (OUD) Training For Providers
Span Class Result Type
Changes take effect on the first day of the month Providers should verify eligibility before every visit by using one of the options below Secure Provider Portal Provider SuperiorHealthPlan 24 7 Interactive Voice Response Line 1 800 218 7453 Provider Services HMO and HMO SNP 1 877 391 5921
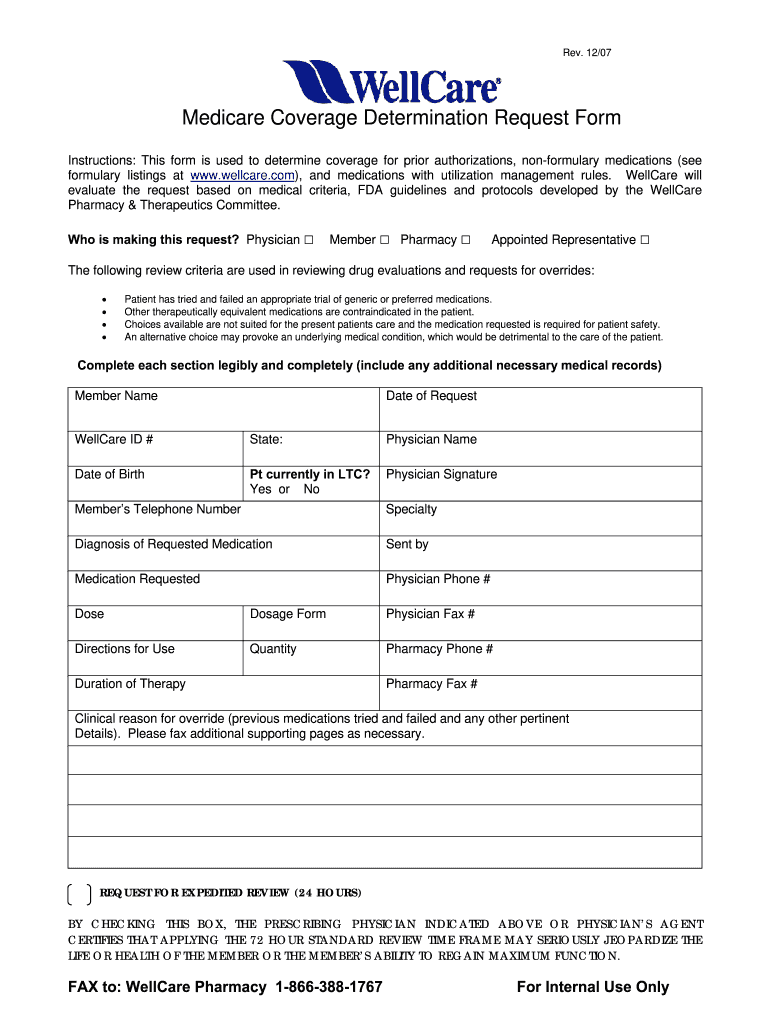
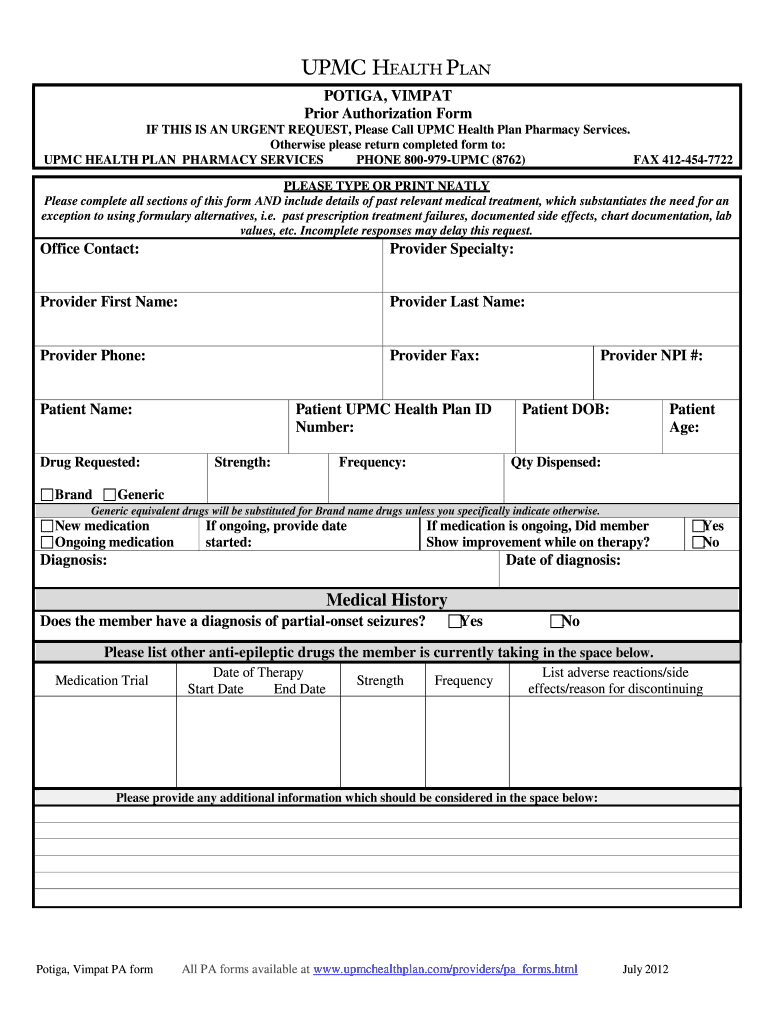
Wellcare Prior Authorization 2007 2023 Form Fill Out And Sign Printable PDF Template SignNow
Covermymeds Humana Prior Auth Form Form Resume Examples bX5aVMLOwW
Allwell Prior Auth Form
Wellcare by Allwell Pre Auth DISCLAIMER All attempts are made to provide the most current information on the Pre Auth Needed Tool However this does NOT guarantee payment Payment of claims is dependent on eligibility covered benefits provider contracts correct coding and billing practices
2024 Information 2023 Information Prior Authorization Rules for Medical Benefits What is Prior Authorization Prior Authorization is a request made by you or your doctor to get Wellcare By Allwell s approval before receiving treatment
Today 39 S Option Prior Auth Forms Fill And Sign Printable Template Online US Legal Forms
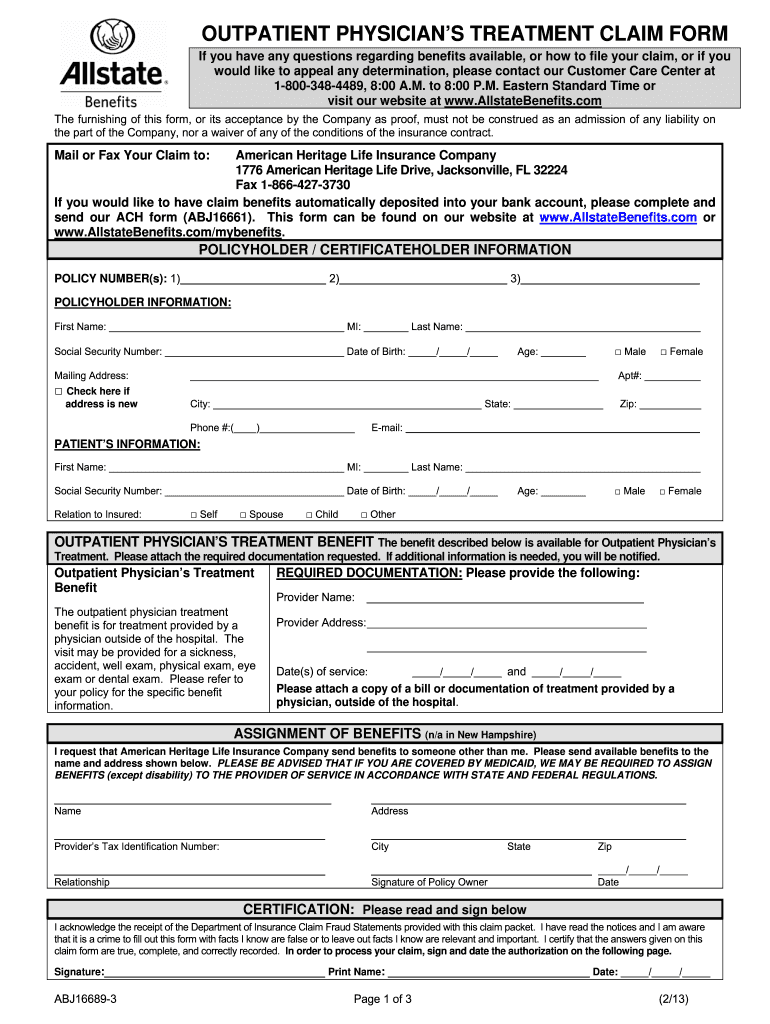
Allstate Wellness Claim 2013 2023 Form Fill Out And Sign Printable PDF Template SignNow

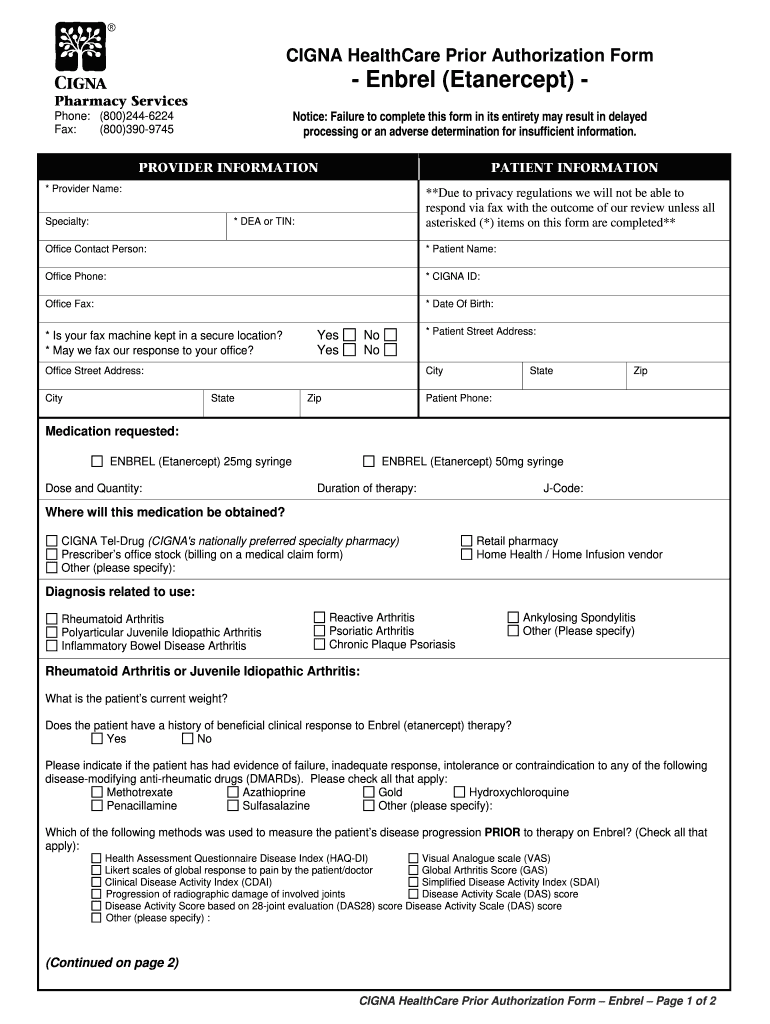
Wellcare Medicare Part D Medication Prior Authorization Form Form Resume Examples A19XB5QRV4
Medicare Authorization Form Fill Online Printable Fillable Blank Gambaran
Covermymeds Humana Prior Auth Form Form Resume Examples bX5aVMLOwW