Blue Cross Blue Shield Of Massachusetts Prior Authorization Form - MASSACHUSETTS STANDARD FORM FOR MEDICATION PRIOR AUTHORIZATION REQUESTS Some plans might not accept this form for Medicare or Medicaid requests For professionally administered medications including buy bill fax to 1 888 641 5355 For BCBSMA employees fax to 1 617 246 4013 E Compound and Off Label Use
Massachusetts Standard Form for Medication Prior Authorization Requests NOTE Some plans might not accept this form for Medicare or Medicaid requests Questions Call our Clinical Pharmacy Operations area at 1 800 366 7778 Tips for using this electronic form Make sure to fill out the form completely and submit it
Blue Cross Blue Shield Of Massachusetts Prior Authorization Form

Blue Cross Blue Shield Of Massachusetts Prior Authorization Form
To request that a printed provider directory, pharmacy directory, formulary, or Evidence of Coverage (EOC) be mailed to you, or if you need help finding these plan documents, please call Member Service at 1-800-200-4255 (TTY: 711) April 1 through September 30, 8:00 a.m. to 8:00 p.m. ET. Monday through Friday, or October 1 through March 31, 8:00 ...
Prior Authorization Pharmacy FAQs Prior Authorization Medication management With input from community physicians specialty societies and our Pharmacy Therapeutics Committee which includes community physicians and pharmacists from across the state we design programs to help keep prescription drug coverage affordable Expand All
Eform Blue Cross Blue Shield Of Massachusetts
If we determine that the services are medically necessary we send an approval or authorization in writing to the member primary care provider PCP the treating physician and the facility if applicable to let them know that we have approved the services When a request for service is not approved we notify the PCP and the member

Blue Cross Blue Shield Overseas Claim Form Fill And Sign Printable Template Online US Legal
DEFINITION OF PRIOR AUTHORIZATION For certain drugs your doctor or health care provider will need to contact us before you fill your prescription The following list of prescription drugs is subject to Prior Authorization
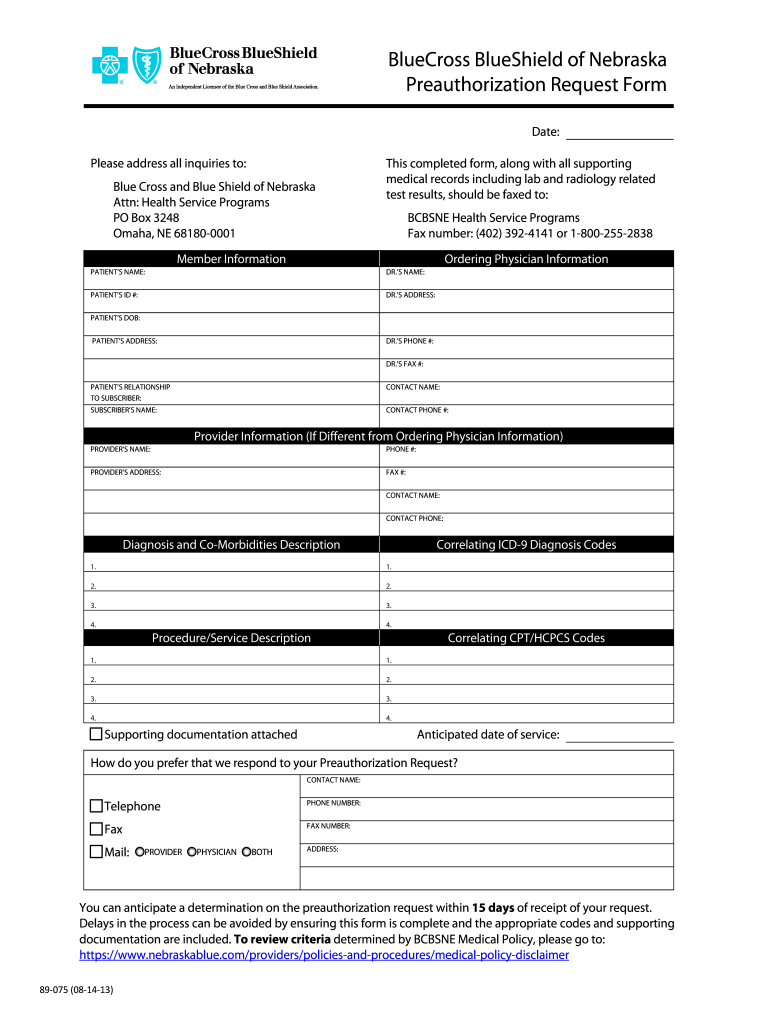
Blue Cross Blue Shield Of Nebraska Prior Authorization Form Fill Out Sign Online DocHub
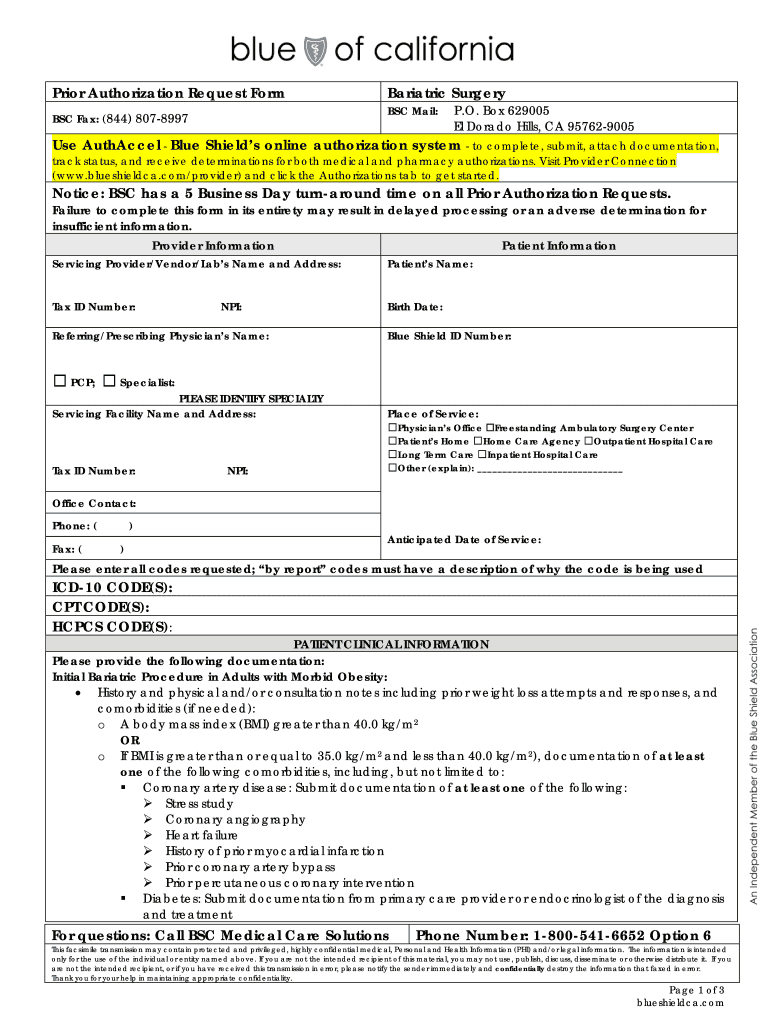
CA Blue Shield Prior Authorization Request Form Bariatric Surgery 2016 2021 Fill And Sign
Span Class Result Type
Habilitation Services Outpatient Rehabilitation Therapy Primary care providers PCPs and designated specialists with an open referral from the PCP can refer a member for short term rehabilitation therapies including Physical therapy Occupational therapy Speech therapy Habilitation Services
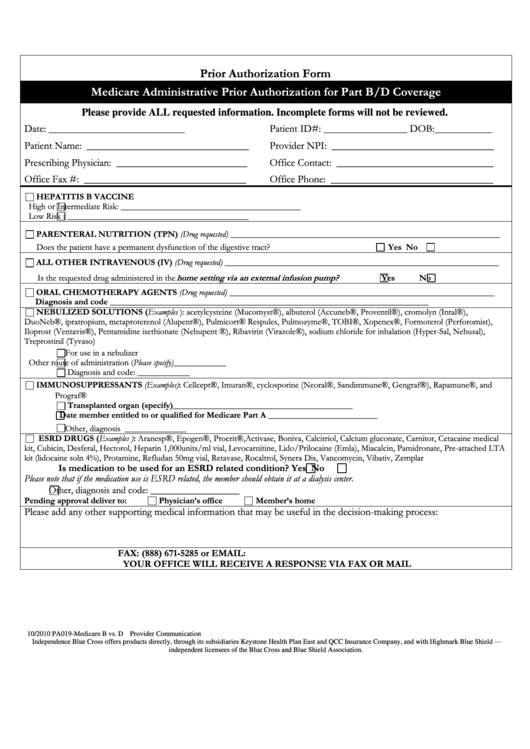
Medicare Administrative Prior Authorization For Part B d Coverage Printable Pdf Download
Prior authorization prior approval Step therapy Formulary quantity limit Non formulary quantity limit Requirements and criteria Prior Authorization Step Therapy Criteria To see a complete list of drugs that require prior authorization or step therapy view the documents below
To download the form you need, follow the links below. Can't view PDF documents? Download Adobe Acrobat®' Reader. Appeals and Grievances Administrative and Privacy Health Plans—Miscellaneous Health and Wellness Member Claims Submission Pharmacy Travel Benefit Reimbursements Tax Forms
Online Forms Plan Documents Blue Cross Blue Shield Of Massachusetts
Authorization Manager available 24 7 is the quickest way to review authorization requirements request authorizations submit clinical documentation check existing case status and view print the decision letter For commercial members the requests must meet medical policy guidelines To ensure the request is processed accurately and quickly
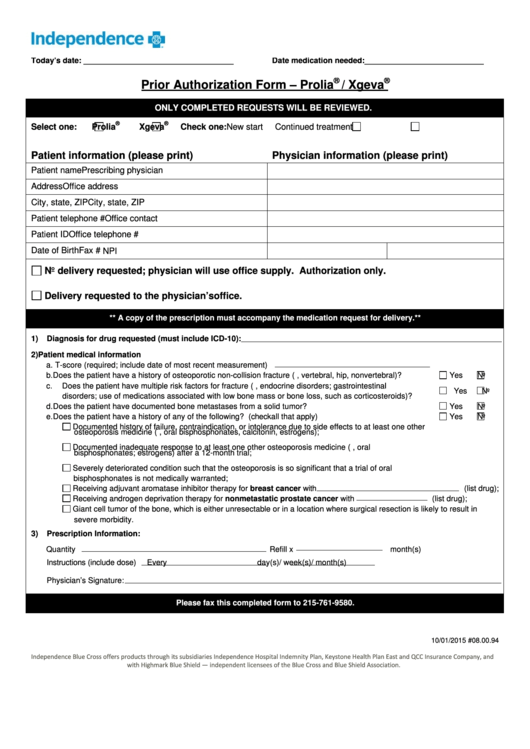
Top 28 Blue Cross Blue Shield Prior Authorization Form Templates Free To Download In PDF Format

Carefirst Blue Cross Blue Shield Federal Claim Form
Blue Cross Blue Shield Of Massachusetts Prior Authorization Form
Prior authorization prior approval Step therapy Formulary quantity limit Non formulary quantity limit Requirements and criteria Prior Authorization Step Therapy Criteria To see a complete list of drugs that require prior authorization or step therapy view the documents below
Massachusetts Standard Form for Medication Prior Authorization Requests NOTE Some plans might not accept this form for Medicare or Medicaid requests Questions Call our Clinical Pharmacy Operations area at 1 800 366 7778 Tips for using this electronic form Make sure to fill out the form completely and submit it
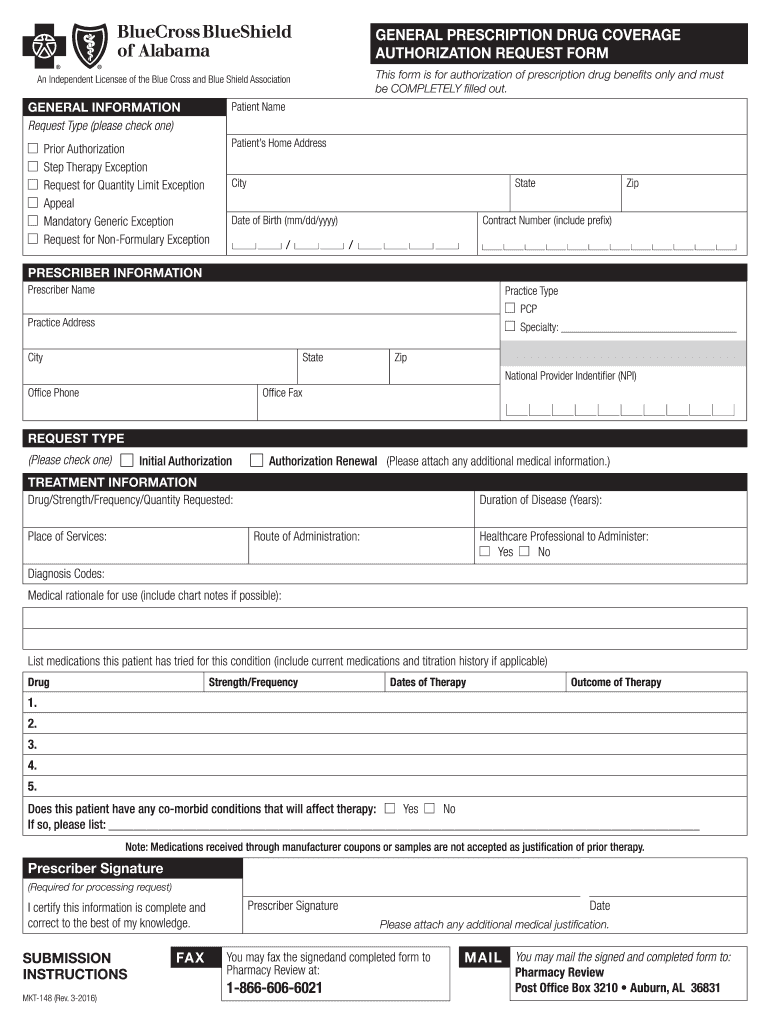
2008 Form AL BCBS MKT 148 Fill Online Printable Fillable Blank PdfFiller

Traitement De La D Pendance La Codeine
Blue Cross Blue Shield Referral Form Printable Printable Forms Free Online
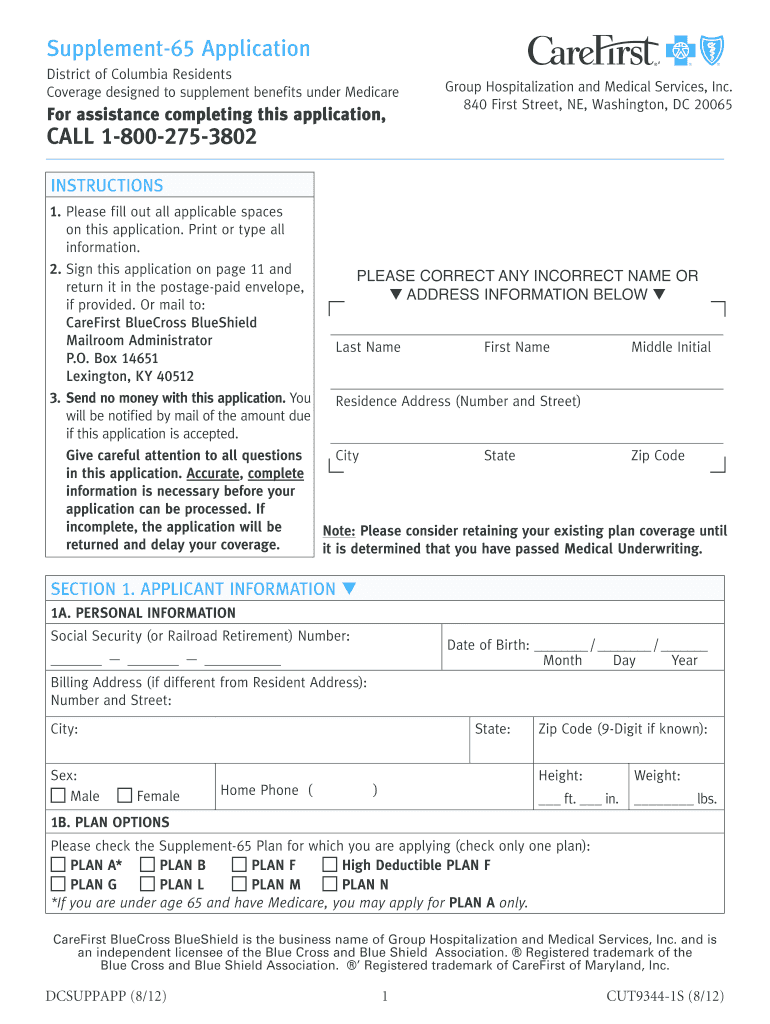
Carefirst Blue Cross Major Medical Claim Form

Mass Standard Pa Form Fill Online Printable Fillable Blank PdfFiller