Initial Psychiatric Soap Note Template - SOAP notes are a helpful method of documentation designed to assist medical professionals in streamlining their client notes Using a template such as SOAP note means that you can capture store and interpret
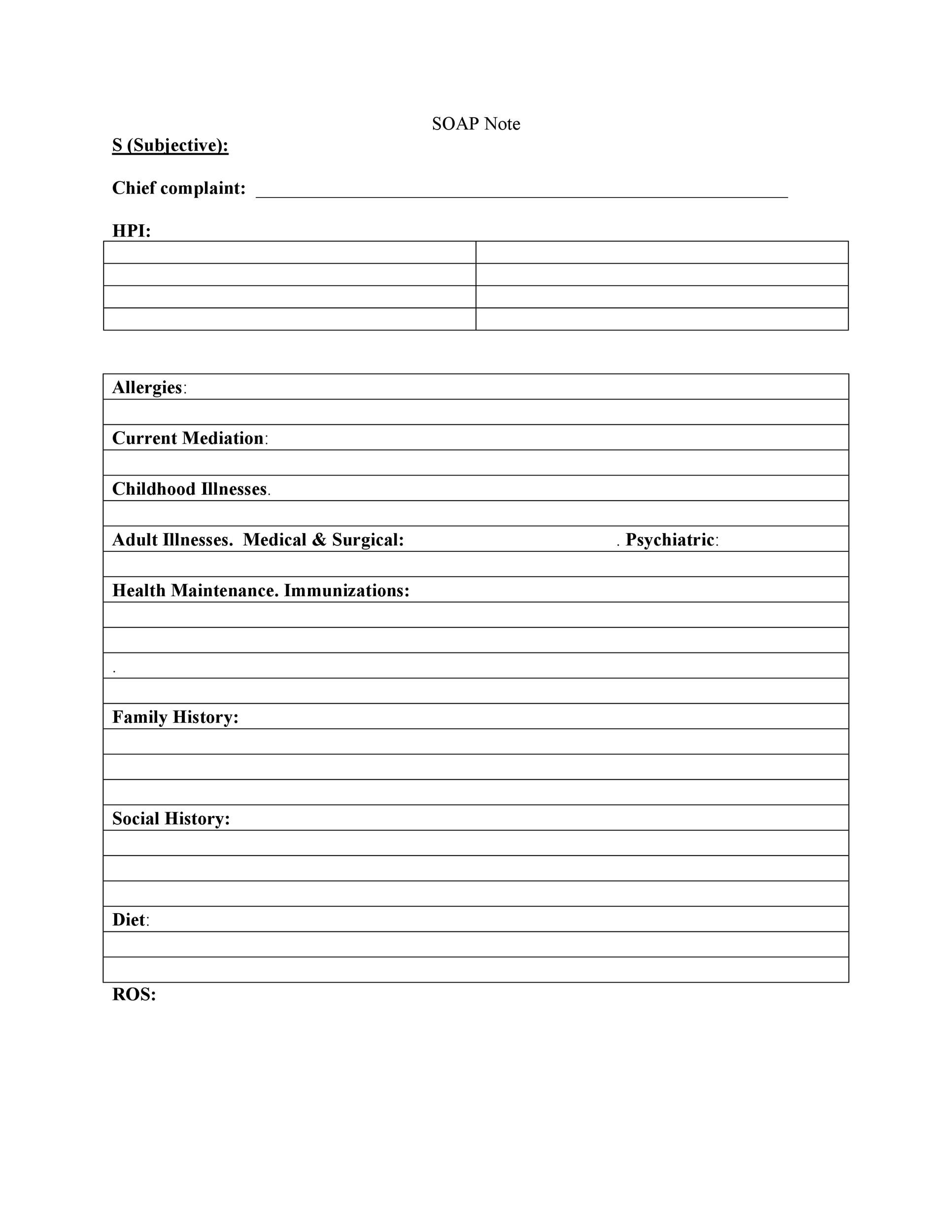
In this post we will review what SOAP notes are how to write a SOAP note tips for effective SOAP notes and a template you can use for your SOAP notes Download Our comprehensive SOAP Note PDF Template for mental health professionals and other medical professionals for easy note taking and digital storage of client notes
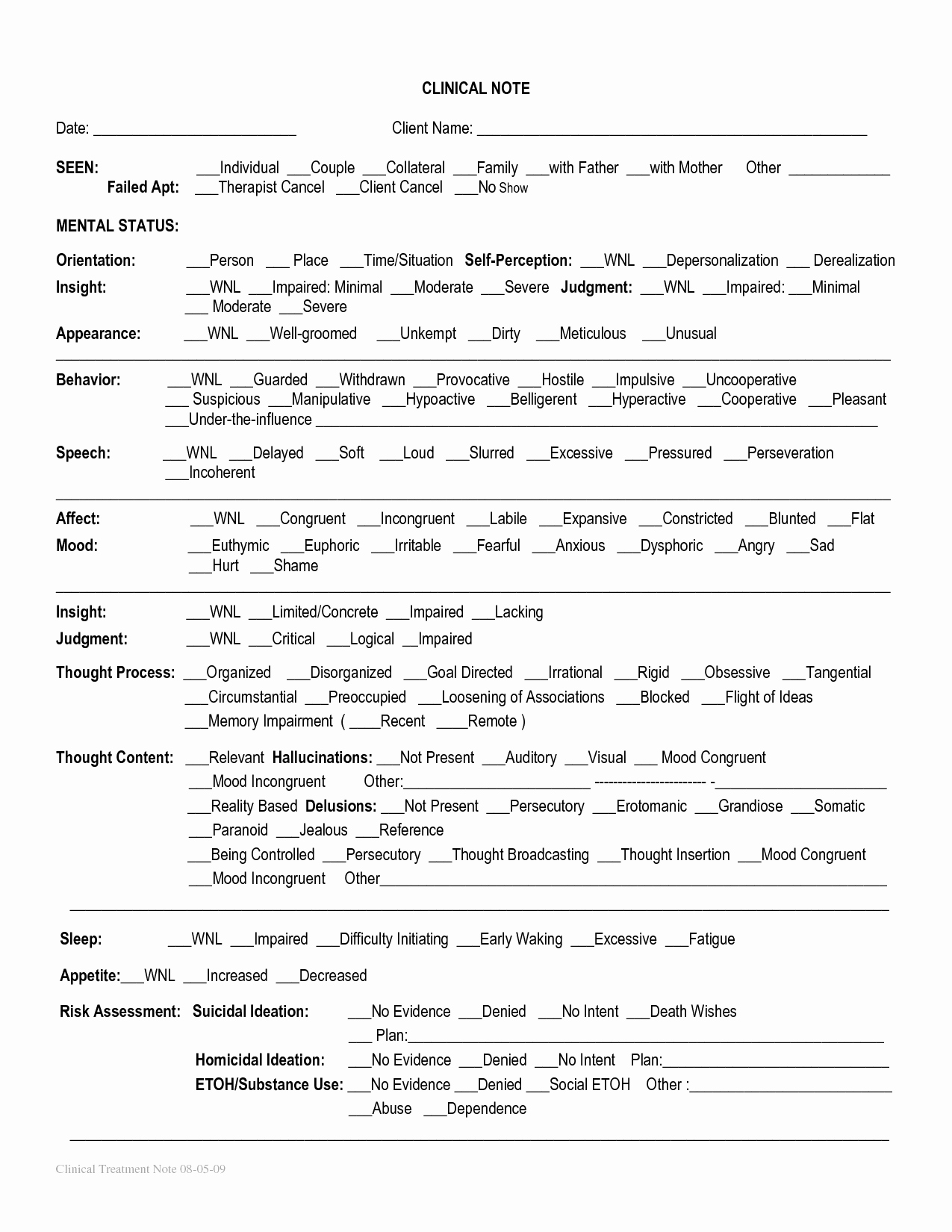
Initial Psychiatric Soap Note Template

Initial Psychiatric Soap Note Template
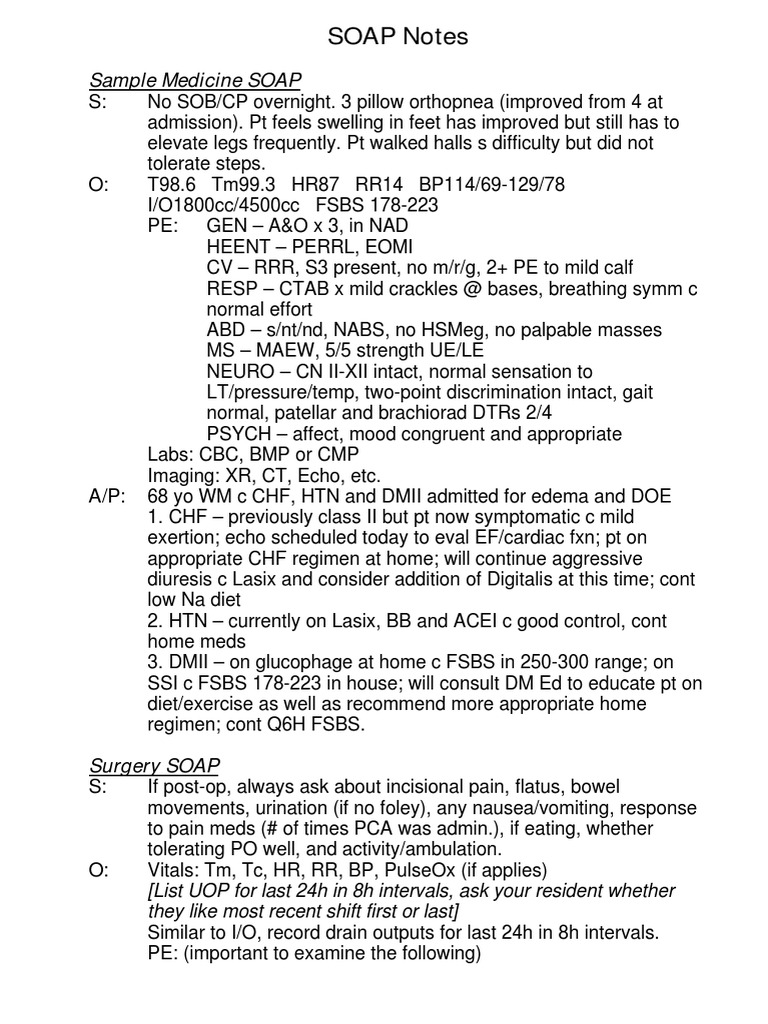
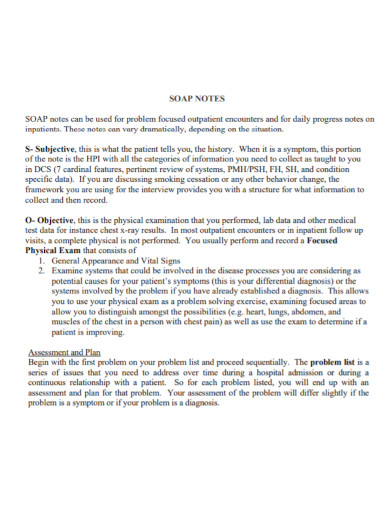
Here’s how to write SOAP notes. Learning how to write a SOAP note can be one of the most effective ways for clinicians to track, assess, diagnose, and treat clients. Here’s how to write SOAP notes. .
HISTORY OF PRESENTING PROBLEM Chief Complaint Date and Time of Service Patient is see in this Intake Followup with psychotherapy for depression anxiety psychosis substance abuse cognitive impairment impulsivity mood lability sleep disturbance alcohol dependence opiate dependence autism spectrum disorder other
Comprehensive SOAP Notes For Counseling Editable PDF Template
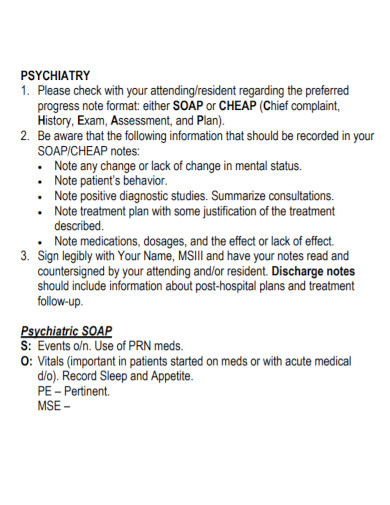
SOAP Subjective Objective Assessment and Plan notes are a structured method for documenting patient information and creating a treatment plan in psychiatric mental health nurse practice This guide provides a thorough overview of SOAP notes their purpose and essential elements tailored for PMHNPs

Physical Therapy Progress Note Template Notes Template Report Template
What Are SOAP Notes Professionals in the medical and psychological fields often use SOAP notes while working with patients or clients They are an easy to understand process of capturing the critical points during an interaction Coaches also can make use of SOAP notes with some adaptations

Pt Soap Note Example 15 SOAP Note Examples And Templates 2023 Update
Printable Soap Note Template Customize And Print
15 SOAP Note Examples And Templates 2023 Update Carepatron
Standardized format The structured format of SOAP notes allows healthcare providers to quickly and easily access pertinent information about a patient s condition and treatment plan 2 Improved communication SOAP notes facilitate clear and concise communication between healthcare providers ensuring continuity of care for the patient 3
29 Psychiatric Soap Note Example Pics Nalo
All other text was created by clicking templated content buttons Visit ICANotes for a free trial or demo PSYCHIATRIC HOSPITAL 2121 Main Street Anywhere USA Date of Exam 4 24 2015 Time of Exam 11 59 56 AM Patient Name Jones January Patient Number 1000010659260 PRE ADMISSION ASSESSMENT Presenting Problem Psychosis
sample text. Comprehensive list of Past psychiatric medications: sample text. Highest dosages and Reasons for discontinuation: Past/present use of Tobacco: (include type, when used, how long used, age began using, what route, tolerance, and withdrawal, last time used, and longest period of abstinence.) sample text.
How To Write SOAP Notes With Template SimplePractice
Sample text Dysthymia 2 out of 6 for at least 2 years Decreased or increased appetite Decreased concentration Hopelessness Decreased energy Worthlessness Sleep disturbances sample text Manic Episode Lasting at least one week or hospitalization was necessary Persistently elevated mood Persistently irritable mood

Initial Psychiatric SOAP Note Template There Are Different Ways docx

Pin On Note Templates
Initial Psychiatric Soap Note Template
All other text was created by clicking templated content buttons Visit ICANotes for a free trial or demo PSYCHIATRIC HOSPITAL 2121 Main Street Anywhere USA Date of Exam 4 24 2015 Time of Exam 11 59 56 AM Patient Name Jones January Patient Number 1000010659260 PRE ADMISSION ASSESSMENT Presenting Problem Psychosis
In this post we will review what SOAP notes are how to write a SOAP note tips for effective SOAP notes and a template you can use for your SOAP notes Download Our comprehensive SOAP Note PDF Template for mental health professionals and other medical professionals for easy note taking and digital storage of client notes

Initial Psychiatric Interview SOAP Note Template IResearchNet
31 How To Write Clinical Impressions WilliamAryen

Sample Soap Note Examples Occupational Therapy Schools Soap Psychiatric
31 How To Write Clinical Impressions WilliamAryen
Psychiatric Soap Note Example Peterainsworth