Uphp Prior Authorization Form - Prior Authorization For prescribers only for questions regarding prior authorization or to initiate prior authorization requests call 1 248 540 6686 General Pharmacy Benefit Information
The goal of the Upper Peninsula Health Plan UPHP is to provide our members rational clinically appropriate and cost effective pharmaceutical care Providers may utilize the prior authorization forms below to request approval of prior authorization or medical necessity reviews Choose the appropriate formulary to obtain detailed coverage
Uphp Prior Authorization Form
Uphp Prior Authorization Form
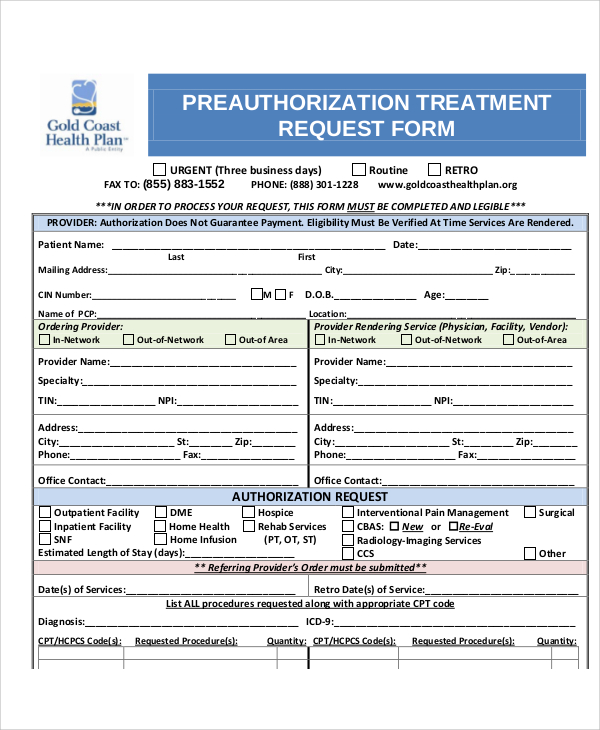
Medicare Part B drugs do not require prior authorization. *Please note that if the ancillary/service provider is not in the UPHP provider network and there is not a current out-of-network authorization, this request will not be reviewed and will be returned to the requesting provider.
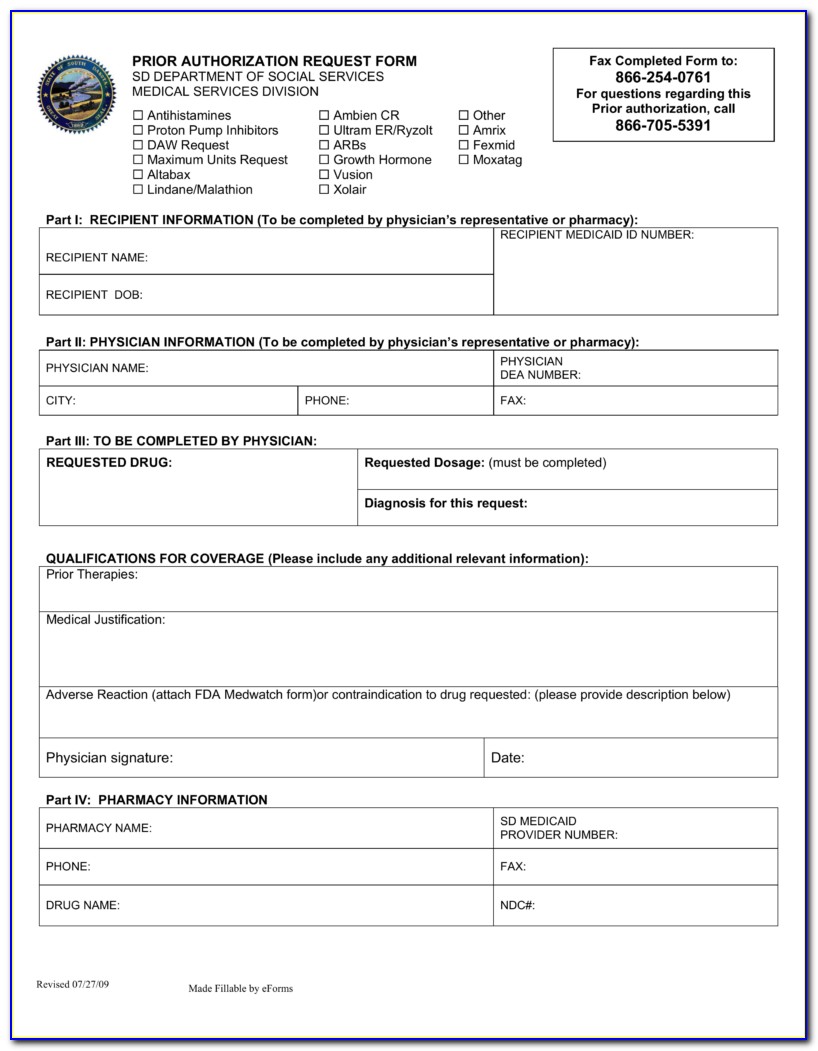
Medicaid Medical Pharmacy J codes are authorized by UPHP please go to see forms on uphp 853 West Washington Street Marquette Michigan 49855 906 225 7500 FAX 906 225 9269 1 800 835 2556 uphp UPHP Prior Authorization Request Form Author UPHP
UPHP
This is called prior authorization This approval from UPHP may be required before you get a service medical equipment or fill a prescription in order to be paid for by UPHP Work with your provider to see if an authorization has been given UPHP provides information to UPHP network providers on what services require prior authorization

A Checklist To Accelerate Prior Authorization Approvals Infographic Infinx
UPHP Upper Peninsula Health Plan is a managed care organization that provides health coverage to eligible residents of Michigan s Upper Peninsula UPHP offers various plans and programs such as Medicare Medicaid MI Health Link and Healthy Michigan Plan UPHP also provides online tools and resources for members providers and pharmacies such as claims submission contact information
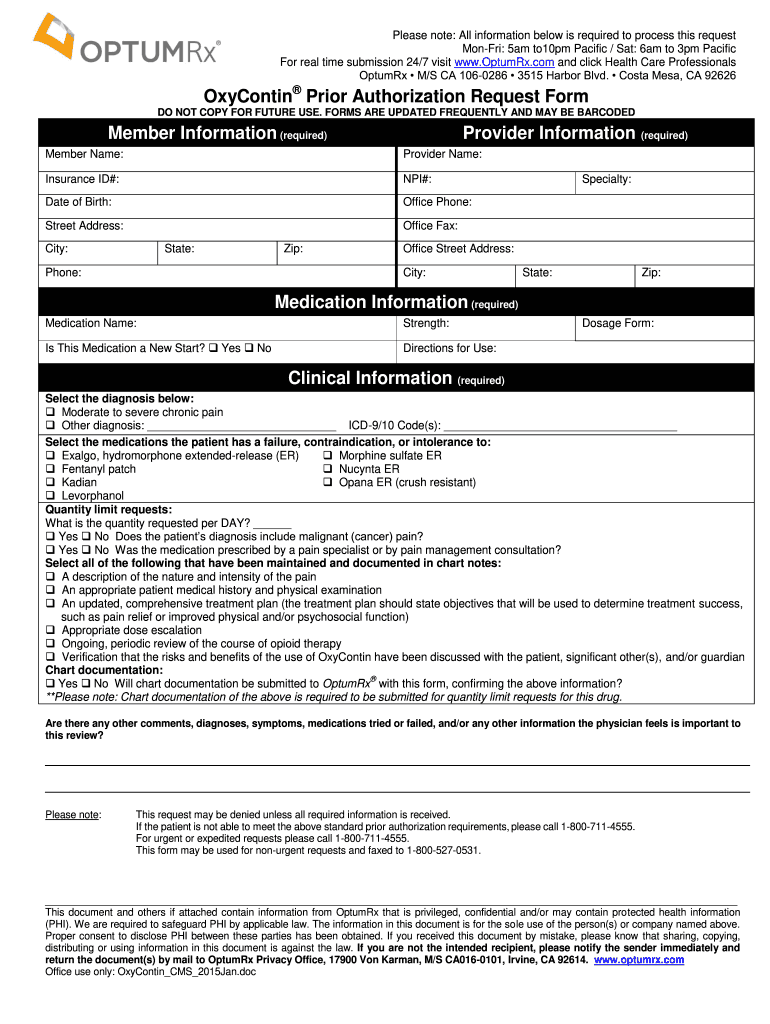
FREE 8 Sample Caremark Prior Authorization Forms In PDF

Ach Payment Authorization Form Template Template 2 Resume Examples 05KADRN1wP
Upper Peninsula Health Plan Medicaid Pharmacy Information
ME Order DME Medical Supply Prior Authorization Request Form Please Include Current Supporting Documentation and a Prescription Order from the Physician No Retrospective Requests UPHP Medicare UPHP Medicaid MI Health Link Member Name UPHP HMP UPHP CSHCS Member ID Number Member Date of Birth Prescribing Physician Name Urgency Standard Expedited member s life health function in serious
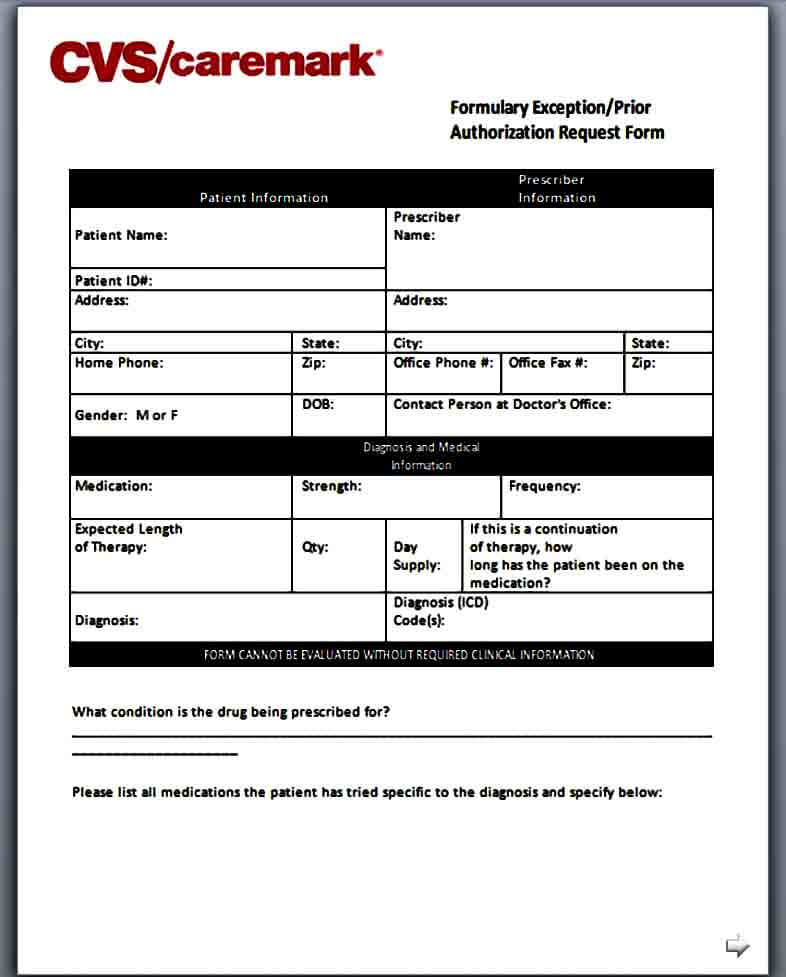
Template Caremark Prior Authorization Form Mous Syusa
A formulary is a list of covered drugs which represents the prescription therapies believed to be a necessary part of a quality treatment program We will generally cover the drugs listed in our formulary as long as the drug is medically necessary the prescription is filled at a network pharmacy and other plan rules are followed
upper peninsula health plan prior authorization form uphp coverage uphp income limits upper peninsula health plan provider enrollment Create this form in 5 minutes!
UPHP
Follow the simple instructions below The preparing of lawful documents can be expensive and time ingesting However with our pre built online templates everything gets simpler Now creating a UPHP PRIOR AUTHORIZATION PA REQUEST FORM FAX TO 906 225 9269 takes no more than 5 minutes
Key covermymeds Prior Authorization Form Form Resume Examples EvkBZWPk2d

UPHP
Uphp Prior Authorization Form
A formulary is a list of covered drugs which represents the prescription therapies believed to be a necessary part of a quality treatment program We will generally cover the drugs listed in our formulary as long as the drug is medically necessary the prescription is filled at a network pharmacy and other plan rules are followed
The goal of the Upper Peninsula Health Plan UPHP is to provide our members rational clinically appropriate and cost effective pharmaceutical care Providers may utilize the prior authorization forms below to request approval of prior authorization or medical necessity reviews Choose the appropriate formulary to obtain detailed coverage
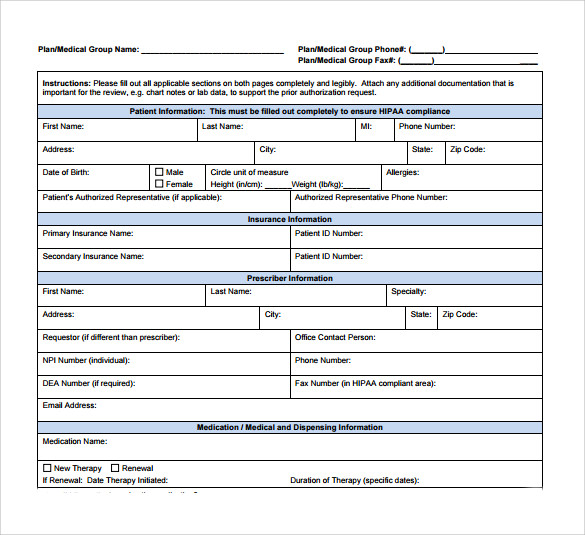
FREE 10 Sample Authorization Request Forms In MS Word PDF
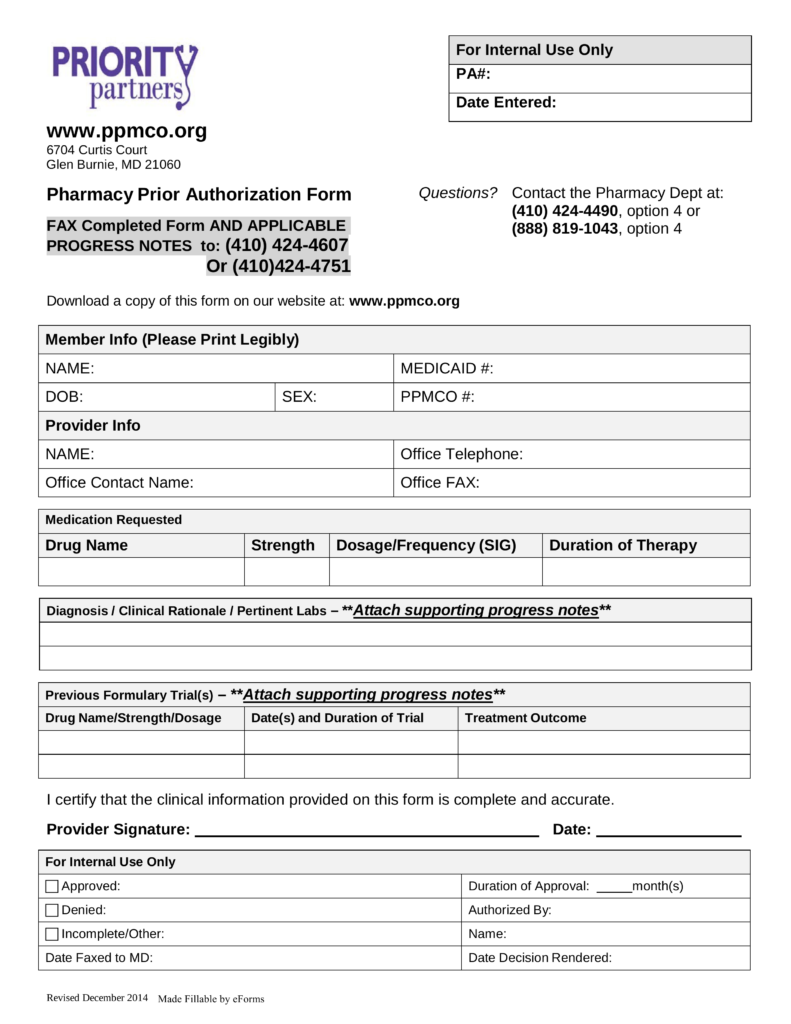
Free Priority Partners Prior Rx Authorization Form PDF EForms
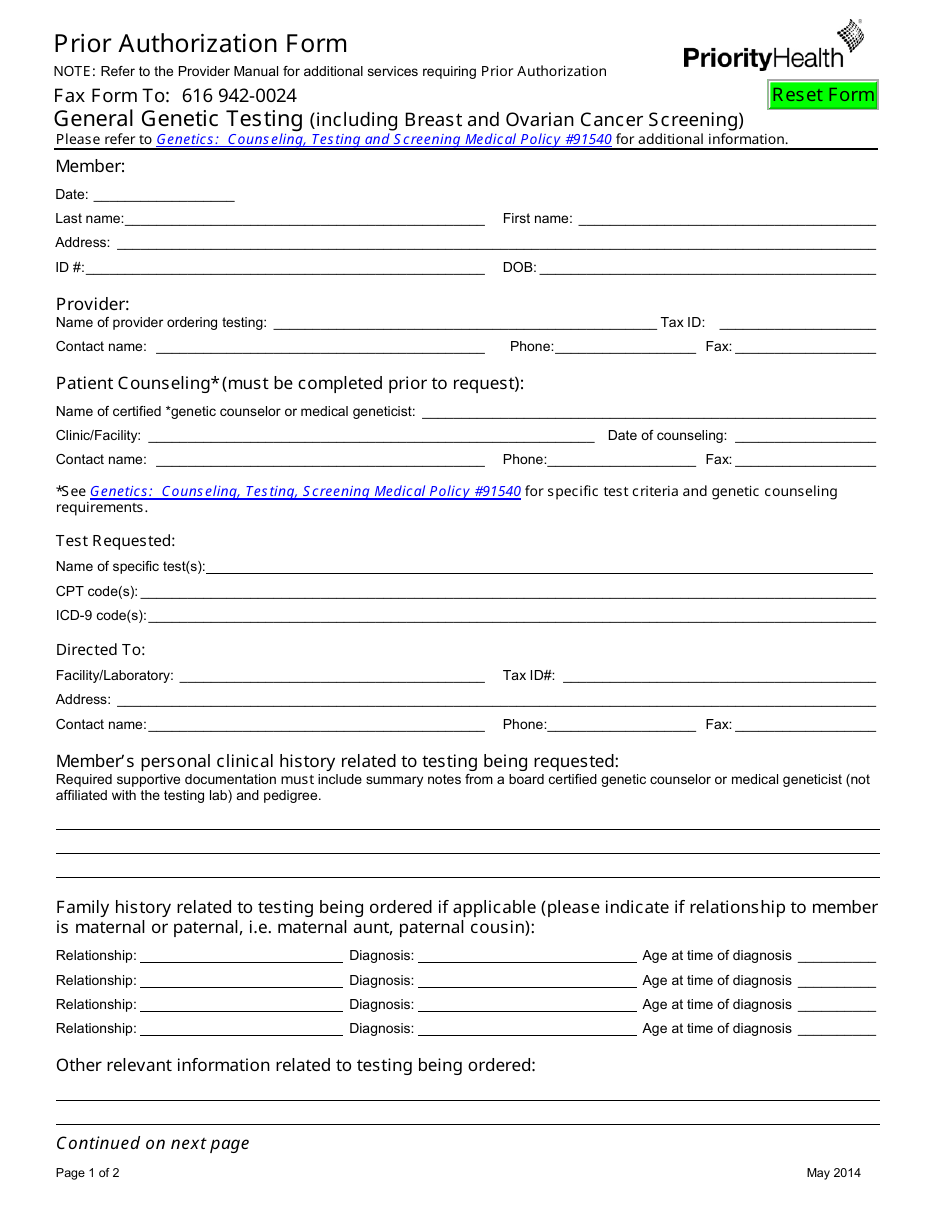
Prior Authorization Form Priorityhealth Fill Out Sign Online And Download PDF Templateroller
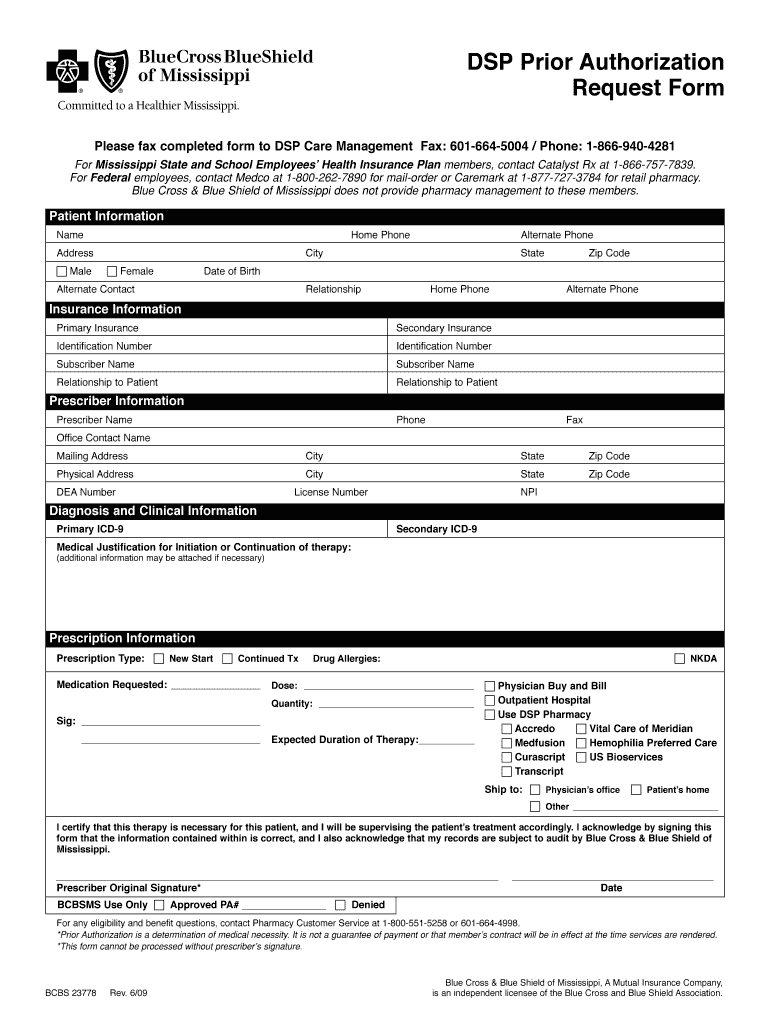
Bcbs Of Mississippi Prior Authorization Form Fill Online Printable Fillable Blank PdfFiller

Is Prior Authorization Process A Burden On Your Practice