Wellcare Appeal Form For Providers - You may file an appeal of a drug coverage decision any of the following ways Online Complete our online Request for Redetermination of Medicare Prescription Drug Denial Appeal Call Refer to your Medicare Quick Reference Guide QRG for the appropriate phone number
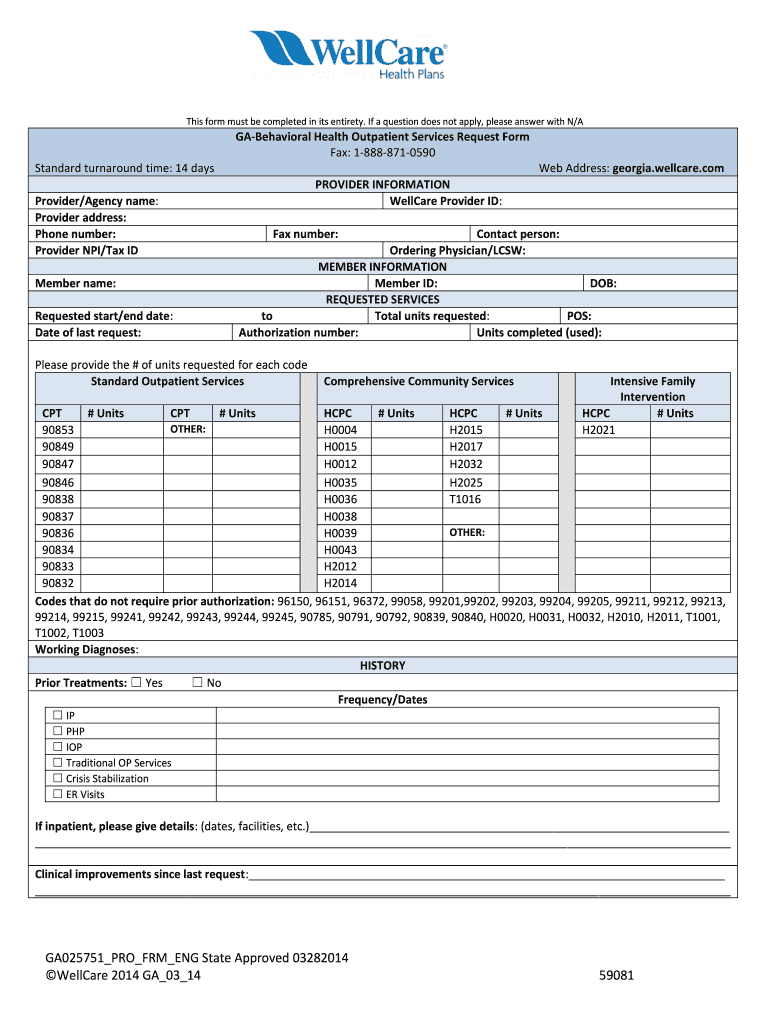
Clinical appeals can be submitted thru our provider portal electronically Primarily address utilization management authorization denials in addition to claim denials related to lack of approved authorizations For these appeals our system will generate a reference number for the submission You may use this reference number to check on the
Wellcare Appeal Form For Providers
Wellcare Appeal Form For Providers
WellCare of North Carolina Attn: Level I - Request for Reconsideration PO Box 5010 Farmington, MO 63640-5010 WellCare of North Carolina Attn: Level II - Claim Dispute PO Box 5000 Farmington, MO 63640-5000
Send this form with all pertinent medical documentation to support the request to Wellcare Health Plans Inc Attn Appeals Department at P O Box 31368 Tampa FL 33631 3368 Your dispute will be processed once all necessary documentation is received and you will be notified of the outcome
Submitting Appeals And Disputes Through The Provider Portal Wellcare
Appointment of Representative Download Provider Payment Dispute Download Provider Reconsideration Request Download Provider Waiver of Liability WOL Download Authorization Forms Delegated Vendor Request Download DME Authorization Request Download Home Health Services Request Download Hospice Authorization Request Download Inpatient Request
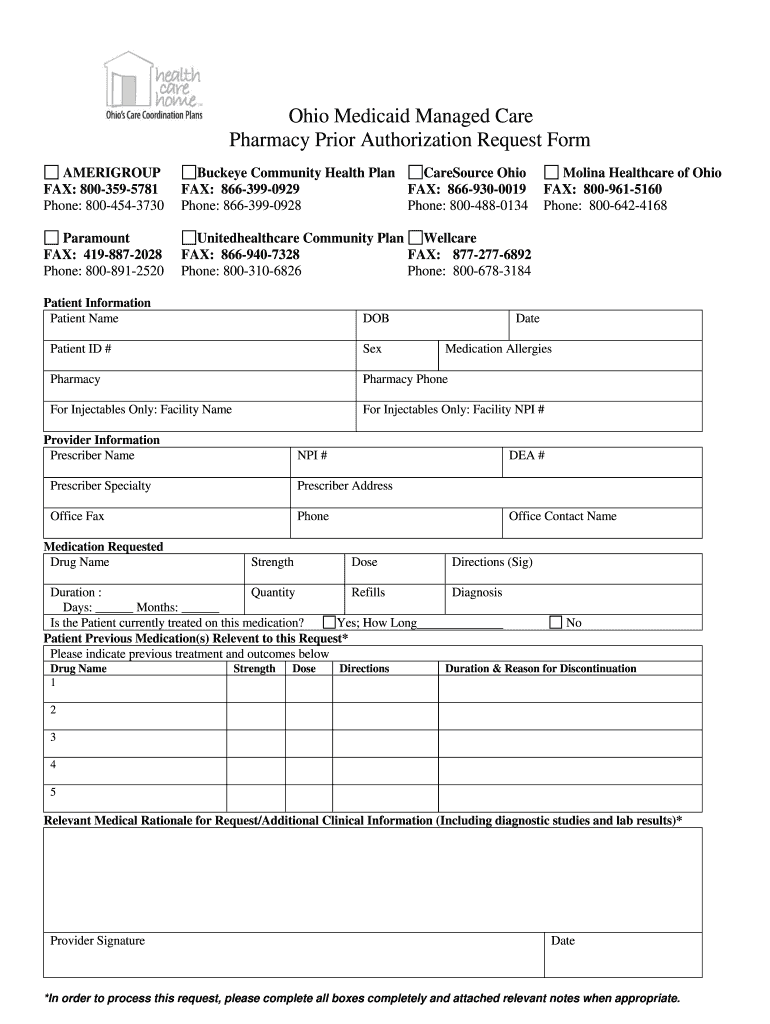
Printable Medicaid Application
Welcome PDP member We have redesigned our website You can now quickly request an appeal for your drug coverage through the Request for Redetermination Form To access the form please pick your state Please select your plan s state to get started Need help We re here for you Contact Us

WellCare The Ascend Advantage Value Based Enrollments VBE
Medicare Appeal Form Cms20027 Medicare United States Medicaid
Coverage Determination Appeal Wellcare
Providers may seek an appeal within 120 calendar days of claims denial Send this form with all pertinent medical documentation to support the request to WellCare Health Plans Inc Attn Appeals Department P O Box 31368 Tampa FL 33631 3368 You may also fax the request if fewer than 10 pages to 866 201 0657
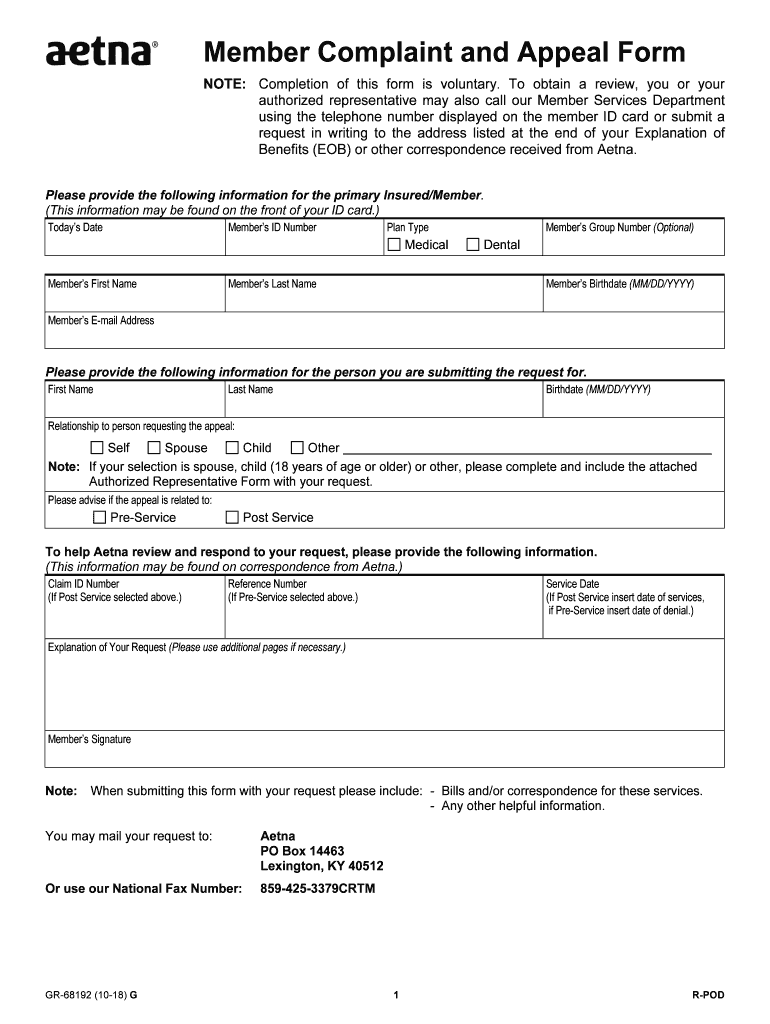
Aetna Appeal 2018 2023 Form Fill Out And Sign Printable PDF Template SignNow
Use this form as part of the Wellcare By Allwell Request for Reconsideration and Claim Dispute process All fields are required information Please Note A Request for Reconsideration Level I is a communication from the provider about a disagreement on how a claim was processed
To appeal an authorization in Denied status, search for the authorization using one of these criteria: Member/Subscriber ID, Provider ID, Patient Name and Date of Birth, Medicare ID or Medicaid ID. Search results will display based on date of service. Select Authorization Appeal from the drop down.
Span Class Result Type
Wellcare By Health Net Health Net Forms and References when submitting an appeal Address for provider disputes and appeals Medicare Provider Disputes PO Box 9030 Farmington MO 63640 9030 21 758g FLY420167EH01w 11 21 Title Provider Appeals Author Health Net Subject FLY420167EH01w 21 758g WCBHN Appeals hires pdf

The Definition Of Skilled Nursing Springpoint Senior Living
WellCare To Transition Pharmacy Benefit Management To CVS Health Beginning Jan 1 2016
Wellcare Appeal Form For Providers
Use this form as part of the Wellcare By Allwell Request for Reconsideration and Claim Dispute process All fields are required information Please Note A Request for Reconsideration Level I is a communication from the provider about a disagreement on how a claim was processed
Clinical appeals can be submitted thru our provider portal electronically Primarily address utilization management authorization denials in addition to claim denials related to lack of approved authorizations For these appeals our system will generate a reference number for the submission You may use this reference number to check on the
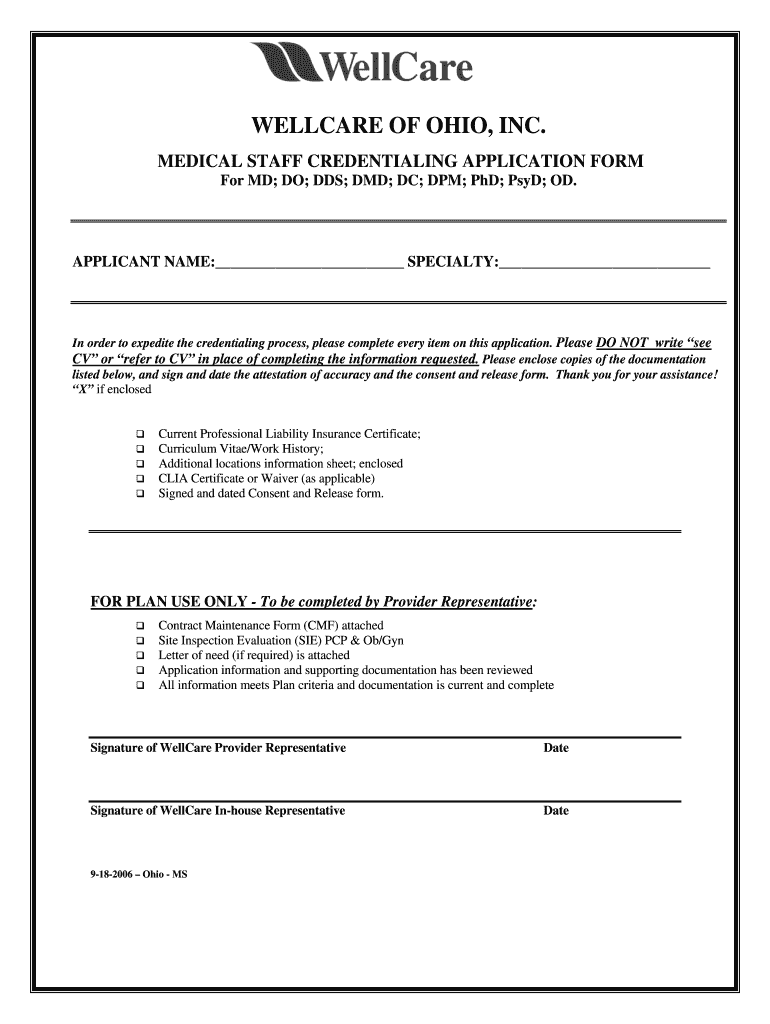
Wellcare Credentialing 2006 2023 Form Fill Out And Sign Printable PDF Template SignNow

Claims My Choice Wisconsin

Wellcare Medicare Part D Coverage Determination Request Form Fill And Sign Printable Template
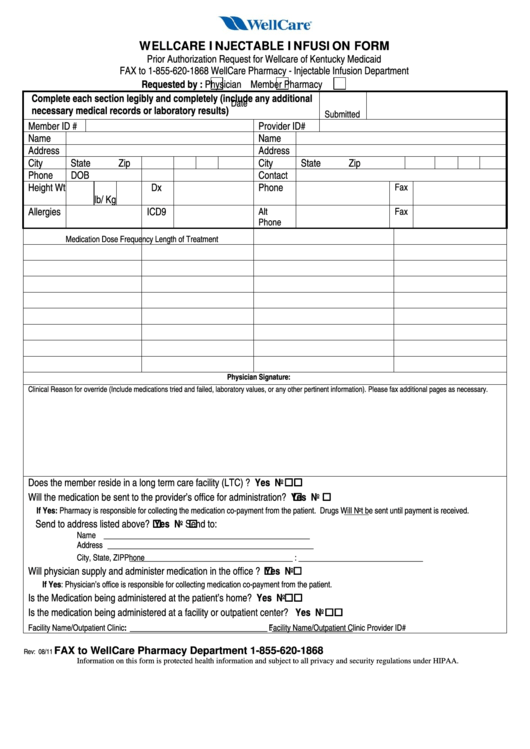
Fillable Wellcare Injectable Infusion Form Prior Authorization Request For Wellcare Of

Valley Health Plan Appeal Form PlanForms

